Have you ever noticed a small, firm bump on your skin that feels a bit like a pebble under your finger? Perhaps it's slightly discolored, or maybe it even feels a little itchy or tender sometimes. While many skin bumps are harmless, one common type that often sparks curiosity (and sometimes concern) is a dermatofibroma. These tiny, tough knots are usually nothing to worry about, but understanding what they are, why they appear, and what your options are if you have one can bring great peace of mind.
This comprehensive guide will take you on a journey to explore everything about dermatofibromas, from their mysterious origins to the various ways they can be managed. We'll dive deep into what causes them, how to recognize them, and the different treatment paths available, helping you feel confident and informed about your skin health.

Imagine a tiny, tough knot just beneath the surface of your skin. That's essentially what a dermatofibroma is! Also known by names like "histiocytoma" or "fibrous histiocytoma," a dermatofibroma is a very common, non-cancerous (benign) skin growth. Think of it as a small, harmless lump made up of extra fibrous tissue and cells called histiocytes.
These growths typically feel firm or hard to the touch, almost like a small stone or a rubber eraser embedded in your skin. They can vary in size, usually ranging from a few millimeters (like a pencil eraser) to about a centimeter (like a blueberry) in diameter. While they can appear anywhere on the body, they are most frequently found on the lower legs, arms, and less commonly, the trunk.
One of the most defining features of a dermatofibroma is something doctors call the "dimple sign." If you gently squeeze the skin around the growth, it often puckers inwards or forms a small dimple, much like a belly button. This happens because the dermatofibroma is slightly tethered or pulled down into the skin. This unique sign can be a helpful clue for doctors when diagnosing these bumps.
Dermatofibromas can also vary in color. They might be pink, red, light brown, dark brown, or even purplish, especially in people with darker skin tones. Sometimes, they can change color over time. While they usually don't cause any problems, some people report that their dermatofibroma feels itchy, tender, or even painful, especially if it's rubbed or bumped frequently.
It's important to remember that dermatofibromas are not dangerous. They are a common skin finding and are generally nothing to worry about. However, because they can sometimes resemble other, more serious skin conditions, it's always a good idea to have any new or changing skin growth checked by a healthcare professional. You can learn more about various skin conditions and when to seek help by visiting resources like The Minor Surgery Center's conditions page at https://www.theminorsurgerycenter.com/conditions.
"Dermatofibromas are benign skin growths, often feeling like a firm knot under the skin, and are known for the characteristic 'dimple sign' when squeezed."

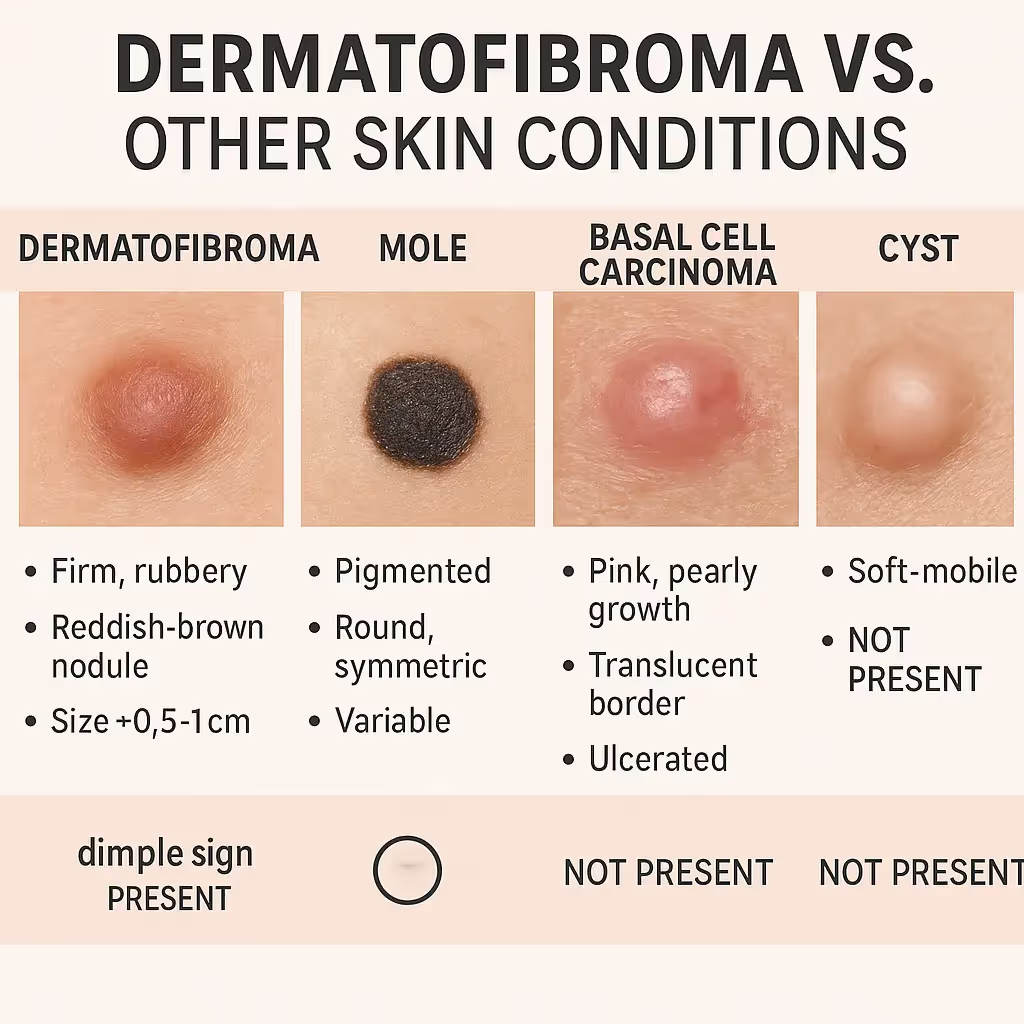
When you find a new bump on your skin, it's natural to wonder what it is. While dermatofibromas are harmless, many other skin conditions can look similar, some of which require immediate medical attention. That's why it's incredibly important not to self-diagnose. A professional evaluation by a dermatologist or a doctor experienced in minor skin procedures is always the safest approach. They have the expertise to tell the difference and ensure you get the right care.
Let's look at how dermatofibromas compare to some other common skin growths:
Here's a quick comparison table to help visualize the differences:
FeatureDermatofibromaMole (Nevus)Basal Cell Carcinoma (BCC)MelanomaCystLipomaFeelFirm, hard, rubberyCan be flat or raised, softPearly, firm, sometimes crustyFlat or raised, often irregularSoft, movable, fluid-filledSoft, doughy, movableAppearanceSmall, round, discolored (pink, brown, red, purple)Uniformly colored (brown, black, tan), symmetricPearly bump, open sore, red patch, scar-likeIrregular shape, varied colors, changingFlesh-colored lump, can be inflamedFlesh-colored lump, under skinDimple SignPresent (often)AbsentAbsentAbsentAbsentAbsentGrowth/ChangeSlow, usually stableStable, but can change over timeSlow but continuous growth, can bleedRapid changes in ABCDEsCan grow, rupture, get infectedSlow growth, stableCancerous?No (Benign)No (but can become melanoma)YesYes (serious)No (Benign)No (Benign)Typical Size0.5 - 1.5 cmVaries widelyVaries widelyVaries widelyVaries widelyVaries widely, often larger
Given the potential for misdiagnosis, it's always best to consult with a healthcare provider. They can properly identify the growth and recommend the appropriate course of action. If you're concerned about a skin lesion, consider reaching out to a clinic like The Minor Surgery Center, which specializes in diagnosing and treating various skin conditions. You can find their contact information at https://www.theminorsurgerycenter.com/contact.
The exact cause of dermatofibromas isn't always perfectly clear, and sometimes they seem to pop up out of nowhere. However, medical experts have identified some common patterns and potential triggers that might lead to their development.
The most widely accepted theory is that dermatofibromas are a reactive process. This means they often form as a response to some kind of minor injury or irritation to the skin. Think of your skin's healing process going a little bit overboard, leading to an overgrowth of fibrous tissue and certain immune cells (histiocytes).
Here are some of the common "injuries" or factors that might spark a dermatofibroma:
It's important to note that not everyone who experiences these minor injuries will develop a dermatofibroma. Many people get insect bites or small cuts all the time without any dermatofibromas forming. This suggests that other factors might play a role, making some individuals more prone to these growths than others.
While dermatofibromas are not considered to be directly inherited, there might be a subtle genetic predisposition in some families. This means that if your parents or close relatives have dermatofibromas, you might have a slightly higher chance of developing them yourself. However, this link is not as strong as it is for some other genetic conditions, and many people develop dermatofibromas with no family history of them.
Dermatofibromas are more commonly seen in adults, particularly in middle-aged individuals. They are less common in children. Women also tend to develop dermatofibromas more frequently than men, though the reason for this difference isn't fully understood.
In rare cases, multiple dermatofibromas (eruptive dermatofibromas) might be associated with certain underlying conditions that affect the immune system, such as:
However, for the vast majority of people, a single dermatofibroma is not linked to any serious underlying health issue and is simply a benign skin finding.
In summary, while the exact "why" can sometimes be elusive, dermatofibromas are most often your skin's slightly overzealous response to a small, forgotten injury. Understanding these potential causes can help demystify these common bumps.
One of the most helpful ways to understand dermatofibromas is to know what they look and feel like. While they can vary slightly from person to person, they share several common characteristics that help doctors identify them.
Dermatofibromas are typically small, round or oval-shaped bumps. Here's a breakdown of their appearance:
Touch is a key part of identifying a dermatofibroma:
While many dermatofibromas are asymptomatic (meaning they don't cause any symptoms), some people do experience:
It's important to remember that these symptoms are usually mild and don't indicate anything serious. However, any new or changing skin lesion, especially one that starts bleeding, growing rapidly, or changing significantly in color, should always be evaluated by a healthcare professional. While we can't show actual images here, searching online for "dermatofibroma images" can give you a visual idea of their varied appearance. Always compare with caution and consult a doctor for a definitive diagnosis.
Diagnosing a dermatofibroma is usually a straightforward process for an experienced healthcare professional, such as a dermatologist, a general practitioner with expertise in skin conditions, or a surgeon specializing in minor procedures. The diagnosis typically involves a combination of visual inspection and tactile examination.
The first step is a thorough visual and physical examination of the skin lesion. Your doctor will look at:
Your doctor will also ask you about the history of the lesion:
In many cases, doctors will use a special handheld device called a dermatoscope. This tool magnifies the skin lesion and illuminates it, allowing the doctor to see structures and patterns within the skin that are not visible to the naked eye.
For dermatofibromas, dermoscopy can reveal characteristic patterns, such as:
These patterns help the doctor confirm the diagnosis without needing more invasive procedures.
While clinical examination and dermoscopy are often enough, there are situations where a skin biopsy might be necessary. A biopsy involves taking a small sample of the skin lesion for examination under a microscope by a pathologist.
A biopsy is typically recommended if:
There are different types of biopsies:
The tissue sample is then sent to a pathology lab. A pathologist, a doctor specialized in diagnosing diseases by examining tissues, will analyze the sample under a microscope. They will look for the characteristic features of a dermatofibroma, such as an overgrowth of fibroblasts (cells that make fibrous tissue) and histiocytes, arranged in a specific pattern. They will also confirm the absence of cancerous cells.
It's crucial to seek professional medical advice for any new or changing skin lesion. As discussed, many skin conditions can look similar, and only a trained eye, sometimes aided by dermoscopy or biopsy, can accurately distinguish between a harmless dermatofibroma and something more serious like melanoma. Early and accurate diagnosis is key for effective treatment, especially for skin cancers. If you have concerns about a skin growth, don't hesitate to reach out to a specialized clinic like The Minor Surgery Center. Their team is equipped to diagnose and manage various skin conditions. You can find more information about their services at https://www.theminorsurgerycenter.com/.
For most people, a dermatofibroma is a harmless growth that doesn't require any treatment at all. Since they are benign (non-cancerous) and don't pose a health risk, the decision to treat one often comes down to personal preference, symptoms, or diagnostic uncertainty.
Here are the main approaches to managing dermatofibromas:
This is the most common approach. If the dermatofibroma is small, not causing any symptoms (like itching or pain), and the diagnosis is clear, many doctors and patients choose to simply leave it alone.
When is observation appropriate?
Benefits of observation:
Drawbacks of observation:
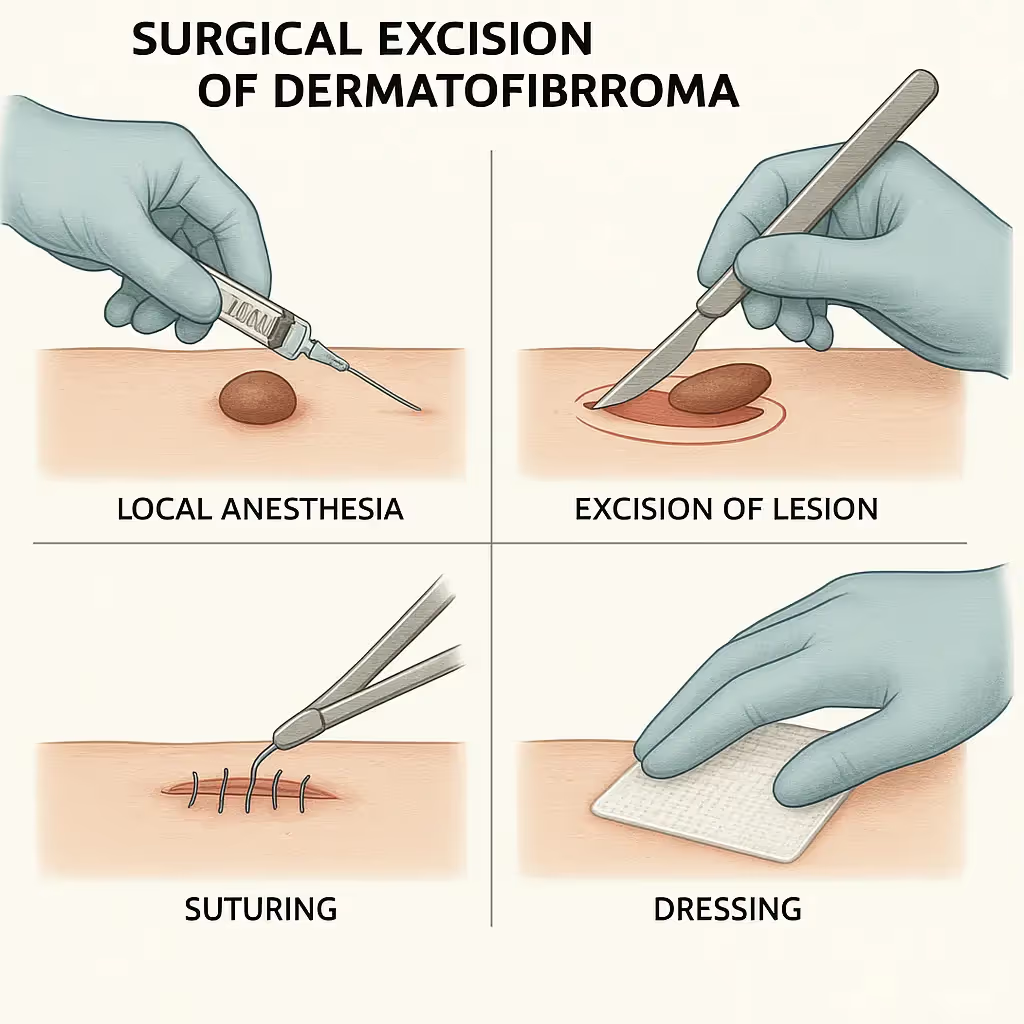
Surgical excision is the most definitive way to remove a dermatofibroma. This procedure involves cutting out the entire lesion using a scalpel.
When is surgical excision recommended?
The Procedure:
Recovery and Scarring:
Benefits of surgical excision:
Drawbacks of surgical excision:
For expertly performed minor surgical procedures, you might consider visiting a specialized clinic. You can learn more about the team and their expertise at https://www.theminorsurgerycenter.com/team.
A shave excision involves using a scalpel to "shave" off the top part of the dermatofibroma, making it flush with the surrounding skin.
When is shave excision considered?
The Procedure:
Recovery and Scarring:
Cryotherapy involves freezing the dermatofibroma with liquid nitrogen. This destroys the cells within the growth.
When is cryotherapy considered?
The Procedure:
Recovery and Scarring:
Certain types of lasers, such as pulsed dye lasers or ablative lasers, can be used to treat dermatofibromas.
When is laser treatment considered?
The Procedure:
Recovery and Scarring:
Injections of corticosteroids directly into the dermatofibroma can sometimes help to flatten it and reduce associated symptoms like itching or tenderness.
When are steroid injections considered?
The Procedure:
Recovery and Scarring:
The choice of treatment depends on several factors: the size and location of the dermatofibroma, the presence of symptoms, cosmetic concerns, the patient's preference, and the doctor's assessment. It's best to discuss all options with your healthcare provider to determine the most suitable approach for you. You can find more information about minor surgical procedures and other conditions treated at https://www.theminorsurgerycenter.com/clinic.
For most people, living with a dermatofibroma is uneventful. Once diagnosed, the primary concern usually shifts from "Is this serious?" to "What do I do about it?" As we've discussed, often the answer is "nothing at all!"
The most important thing to remember about dermatofibromas is that they are benign. This means:
This understanding can significantly reduce anxiety for those who have them. Many people have dermatofibromas for years or even their entire lives without any issues.
"Rest easy: Dermatofibromas are benign skin growths that do not pose a cancer risk."
While dermatofibromas are generally stable, it's always wise to be aware of your skin and consult a doctor if you notice any changes in any skin lesion, including a presumed dermatofibroma. This is not because the dermatofibroma itself is likely to become cancerous, but rather because another, more serious lesion could potentially develop near it, or an initial diagnosis might need re-evaluation.
See a doctor if your dermatofibroma:
These are general guidelines for any skin lesion and are particularly important to consider when monitoring something you've been told is a benign dermatofibroma. When in doubt, a quick check-up can provide reassurance.
For some individuals, the cosmetic appearance of a dermatofibroma can be a source of self-consciousness or discomfort, especially if it's on a highly visible area like the face, neck, or lower legs. While medical necessity might not dictate removal, personal well-being often does.
If a dermatofibroma is impacting your self-esteem, discuss this openly with your doctor. As outlined in the "Treatment Options" section, there are various methods, from surgical removal to laser treatments, that can address cosmetic concerns. Weigh the potential benefits of removal against the possibility of a scar, and make an informed decision that feels right for you.
While dermatofibromas themselves aren't directly linked to sun exposure in the way skin cancers are, good general skin care and sun protection are always important for overall skin health.
Living with a dermatofibroma is usually straightforward. It's about understanding what it is, knowing when to monitor it, and deciding if its presence warrants removal for your comfort or peace of mind. For ongoing skin health questions, exploring resources like the blog at https://www.theminorsurgerycenter.com/blog can be beneficial.
Given that the exact cause of dermatofibromas isn't fully understood, and they often arise from seemingly minor, everyday skin irritations, complete prevention isn't entirely possible. However, understanding the potential triggers can help you take some reasonable steps to reduce your risk, or at least minimize the factors that might contribute to their formation.
Since dermatofibromas are thought to be a reactive growth to skin injury, the most logical prevention strategies revolve around protecting your skin from trauma and ensuring proper wound care.
If you do get a minor cut, scrape, or puncture wound, proper wound care can help promote healthy healing and potentially prevent an overgrowth of fibrous tissue.
If you have conditions that lead to frequent skin irritation or inflammation, such as severe acne or eczema, managing these effectively might indirectly reduce the chance of dermatofibroma formation in those areas.
Ultimately, while you can take steps to protect your skin, dermatofibromas are often just a part of the body's sometimes overzealous healing process. The best approach is to be aware of your skin, practice good skin care, and consult a doctor if you have any concerns about new or changing growths.
It's natural to have questions about skin growths, especially if you've just discovered one. Here are some of the most common questions people ask about dermatofibromas:
A: No, dermatofibromas are not dangerous. They are benign (non-cancerous) skin growths. They do not spread to other parts of the body, and they do not turn into cancer. This is one of the most reassuring facts about them!
A: No, a dermatofibroma itself cannot turn into skin cancer. It's a stable, benign growth. However, because some early skin cancers (like melanoma) can sometimes look similar, it's always important to have any new or changing skin lesion checked by a doctor to ensure an accurate diagnosis.
A: Very rarely. Once a dermatofibroma forms, it typically remains on the skin indefinitely. While some might become less noticeable over many years, they generally do not disappear completely without treatment.
A: The removal procedure itself is not painful because the area is numbed with local anesthesia. You might feel a slight sting from the anesthetic injection, but after that, you should only feel pressure, not pain. After the procedure, you might experience some mild soreness or discomfort as the anesthesia wears off, which can usually be managed with over-the-counter pain relievers.
A: If a dermatofibroma is surgically excised, you will have a linear scar. The appearance of the scar depends on the size and location of the dermatofibroma, your individual healing process, and the surgical technique used. For dermatofibromas, the scar can sometimes be more noticeable than other types of scars because the growth is often tethered deeply in the skin. Shave excisions usually leave a flatter, lighter-colored mark. Cryotherapy or laser treatment may result in a lighter patch of skin (hypopigmentation) or some redness.
A: Yes, recurrence is possible, especially with less invasive methods like shave excision, cryotherapy, or laser treatment, as these methods may not remove the entire growth from its deeper roots. With complete surgical excision, recurrence is less common but can still occur in rare instances.
A: While most people only have one or a few dermatofibromas, some individuals can develop multiple ones. This is usually just a tendency of their skin to form these growths. In very rare cases, multiple eruptive dermatofibromas might be associated with certain underlying health conditions that affect the immune system, but this is uncommon. If you have many dermatofibromas appearing rapidly, it's worth discussing with your doctor.
A: Yes, they can. While many dermatofibromas are asymptomatic, some people experience itching (pruritus) or tenderness, especially if the lesion is frequently rubbed by clothing or jewelry, or if it's located in an area of friction. If symptoms are bothersome, removal might be considered.
A: Absolutely not. Attempting to remove a dermatofibroma yourself can lead to infection, significant scarring, bleeding, and incomplete removal, which could make future professional treatment more difficult. More importantly, you might misdiagnose the lesion, potentially delaying diagnosis and treatment for a more serious condition. Always consult a healthcare professional for any skin concerns.
For more general questions about skin health and minor procedures, you might find helpful information in the FAQs section of a specialized clinic like The Minor Surgery Center at https://www.theminorsurgerycenter.com/faqs.
While dermatofibromas are harmless, knowing when to seek professional medical advice for any skin lesion is crucial for your peace of mind and overall health. It's always better to be safe than sorry when it comes to your skin.
You should definitely see a doctor if:
A healthcare professional, such as a dermatologist or a doctor specializing in minor skin procedures, can accurately diagnose your skin lesion through visual examination, dermoscopy, or if necessary, a biopsy. They can then advise you on the best course of action, whether that's observation, removal, or further investigation.
Don't delay seeking medical attention for any concerning skin changes. Early detection and diagnosis are key for many skin conditions, particularly skin cancers. To schedule a consultation or learn more about skin condition evaluations, visit a trusted clinic's website, such as The Minor Surgery Center, at https://www.theminorsurgerycenter.com/contact.
This interactive tool is designed to help you understand common characteristics of dermatofibromas. It is for informational purposes only and does not replace professional medical advice. Always consult a doctor for a definitive diagnosis and treatment plan.
Dermatofibromas are incredibly common, usually harmless skin growths that many people will encounter at some point in their lives. While their exact cause can be a bit mysterious, they are often a benign reaction to minor skin injury. They are characterized by their firm, rubbery feel and the distinctive "dimple sign" when squeezed.
The most important takeaway is that dermatofibromas are not cancerous and do not pose a serious health risk. For many, simply knowing what they are is enough, and no treatment is needed. However, if a dermatofibroma is itchy, painful, or a cosmetic concern, various safe and effective removal options are available, from surgical excision to cryotherapy.
Remember, while this guide provides comprehensive information, it is not a substitute for professional medical advice. If you have any new, changing, or concerning skin lesions, or if you simply want a definitive diagnosis for peace of mind, always consult a qualified healthcare professional. They can accurately assess your skin and recommend the best course of action for your individual needs. Your skin is your body's largest organ – take good care of it!