Imagine looking in the mirror one day and noticing a hard, horn-like projection growing from your skin. While it might sound like something from a medical mystery, cutaneous horns are real—and more common than you might think. These unusual growths can appear suddenly, causing understandable concern and raising important questions about what's happening beneath the surface of your skin.
A cutaneous horn is a striking skin lesion that resembles a miniature animal horn, often appearing cone-shaped and protruding from the skin's surface. While the growth itself might look alarming, understanding what causes these formations and when to seek treatment can help you make informed decisions about your skin health.
A cutaneous horn (also called cornu cutaneum) is a clinical term describing a specific type of skin lesion rather than a diagnosis itself. The growth consists of compacted keratin—the same protein that makes up your hair and nails—that projects above the skin's surface in a cone or horn shape.
These distinctive growths share several common features:
The term "cutaneous horn" describes the appearance of the growth, not what's causing it. Think of it as a symptom rather than a disease—the visible horn is just the tip of the story, while the real concern lies in what's happening at the base.
While exact prevalence is difficult to determine, cutaneous horns are relatively uncommon. They typically affect:
Location matters when it comes to cutaneous horns. These growths show a strong preference for sun-exposed areas of the body, which provides an important clue about their underlying causes.
Body AreaFrequencyRisk FactorsFaceVery CommonDirect sun exposure, facial skin agingEarsCommonOften overlooked during sun protectionForearms and HandsCommonCumulative sun damage over decadesScalp (balding areas)ModerateUnprotected exposure in those with hair lossNoseModerateProminent position, high UV exposureLower LegsLess CommonMore frequent in women
🔍 Important Note: Cutaneous horns appearing on the penis, vulva, or other genital areas, while rare, have a higher association with underlying malignancy and require immediate medical evaluation.
The sun-exposed pattern of these growths reinforces the critical role that ultraviolet (UV) radiation plays in their development. Areas that receive years of accumulated sun damage are far more likely to develop not just the horn itself, but also the underlying skin changes that cause it.
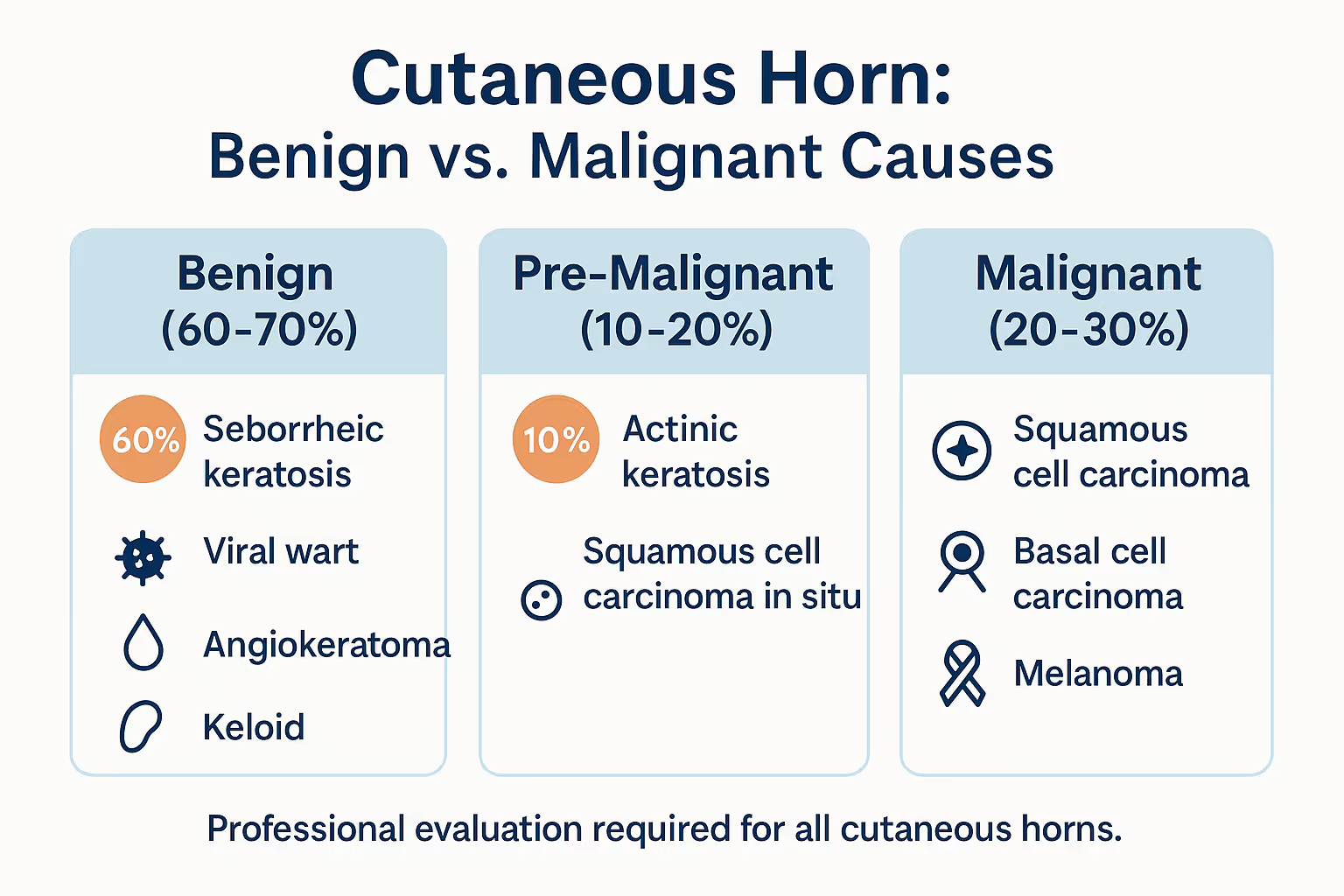
Here's where things get interesting—and medically important. A cutaneous horn isn't a single condition but rather a reaction to various underlying skin issues. The horn you see is actually excessive keratin production triggered by changes in the skin beneath it.
Cutaneous horns can develop on top of benign, pre-malignant, or malignant skin lesions. Understanding what's at the base is crucial for proper treatment.
Seborrheic Keratosis These common, harmless skin growths are one of the most frequent causes of cutaneous horns. They're often described as "barnacles" on the skin and become more common with age.
Viral Warts Human papillomavirus (HPV) can cause warts that occasionally develop into horn-like projections, particularly on the hands and feet.
Molluscum Contagiosum This viral skin infection can sometimes produce a horn-like appearance, especially in immunocompromised individuals.
Keratoacanthoma These rapidly growing dome-shaped growths can develop horn-like centers. While technically benign, they can be difficult to distinguish from skin cancer and often require removal.
Actinic Keratosis These rough, scaly patches result from years of sun damage and are considered pre-cancerous. When they develop into cutaneous horns, careful monitoring and treatment become essential.
Bowen's Disease This is squamous cell carcinoma in situ—essentially an early-stage skin cancer that hasn't yet invaded deeper layers. It requires prompt treatment to prevent progression.
Squamous Cell Carcinoma This common skin cancer is the most frequent malignant cause of cutaneous horns. The cancer cells at the base trigger excessive keratin production, forming the horn.
Basal Cell Carcinoma Less commonly, this most common type of skin cancer can present with a cutaneous horn.
Melanoma Rarely, melanoma—the most dangerous skin cancer—can present with horn-like features, though this is uncommon.
Regardless of the underlying cause, the mechanism is similar:
Think of it like a 3D printer gone haywire—instead of producing a normal, flat layer of skin cells, the affected area keeps building upward, creating the distinctive horn shape.
Understanding your risk factors can help you take preventive measures and know when to seek evaluation. Several factors significantly increase the likelihood of developing a cutaneous horn.
☀️ Chronic Sun Exposure This is the single most important risk factor. Decades of UV radiation damage the skin's DNA, leading to the abnormal cell growth that underlies most cutaneous horns.
👴 Advanced Age The risk increases significantly after age 60, reflecting the cumulative effects of sun exposure and natural skin aging processes.
🧬 Fair Skin (Fitzpatrick Types I-II) People with light skin, blonde or red hair, and blue or green eyes have less natural protection against UV radiation and face higher risk.
🏜️ Geographic Location Living in sunny climates or at high altitudes where UV radiation is more intense increases exposure and risk.
💼 Outdoor Occupation or Recreation Farmers, construction workers, sailors, and outdoor sports enthusiasts accumulate more sun exposure over their lifetimes.
"The majority of cutaneous horns develop on skin that's been damaged by years of sun exposure. Prevention starts with sun protection—it's never too early or too late to start."
Most cutaneous horns develop slowly and cause minimal symptoms beyond their unusual appearance. However, certain features warrant closer attention and prompt medical evaluation.
Visual Characteristics:
Associated Symptoms:
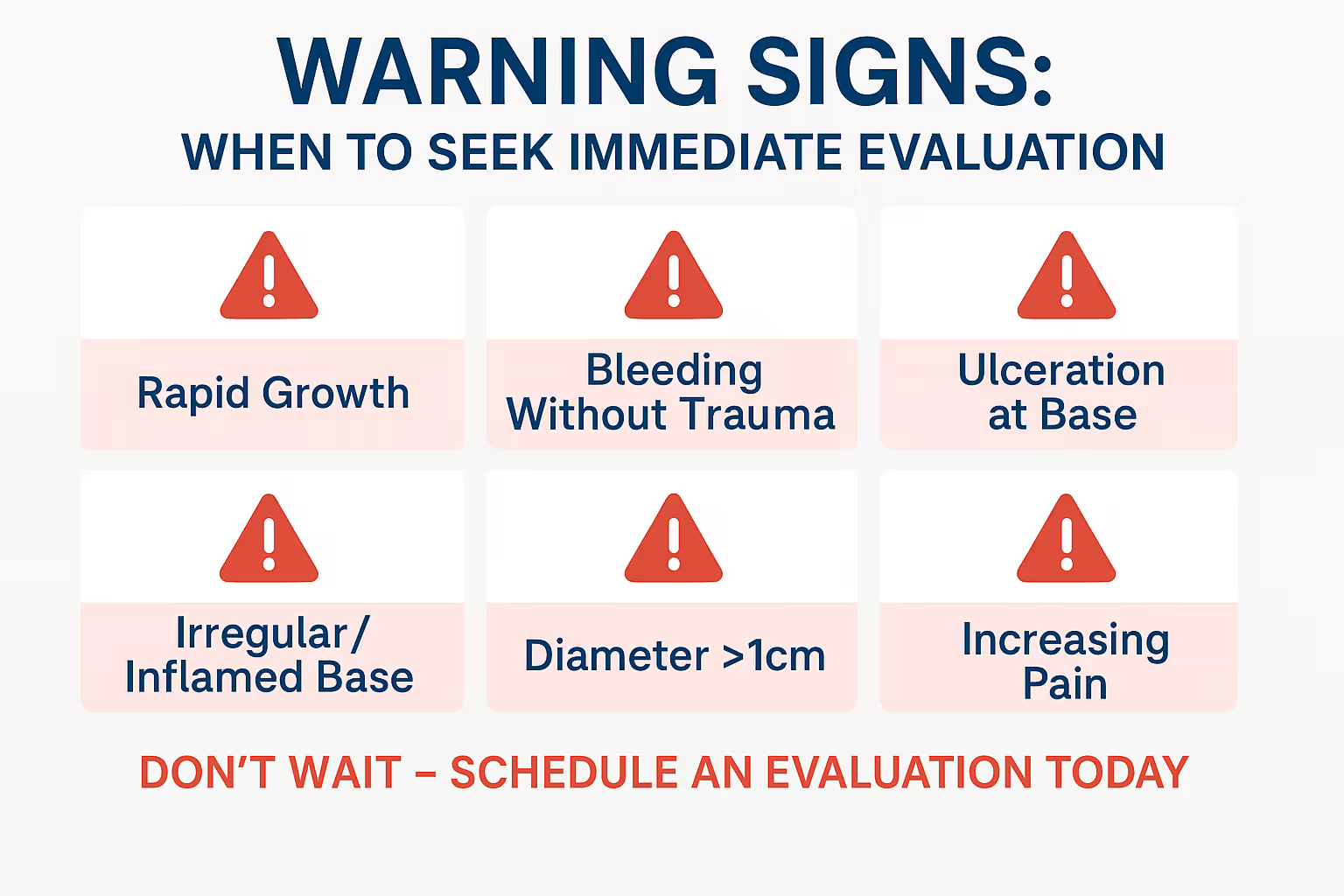
Certain features suggest a higher likelihood of underlying malignancy and require prompt assessment by a healthcare professional:
🚨 Red Flags:
If you notice any of these warning signs, don't wait—schedule an evaluation with a qualified healthcare provider. At The Minor Surgery Center, our experienced team can assess concerning skin growths and provide expert guidance on the next steps.
Proper diagnosis of a cutaneous horn involves more than just looking at the visible growth. A thorough evaluation examines both the horn itself and, critically, what lies beneath it.
Your healthcare provider will begin with a detailed visual inspection:
Many providers use a dermatoscope—a specialized magnifying device with lighting—to examine the structure of the lesion more closely. This non-invasive tool can reveal features invisible to the naked eye and help guide the decision about removal.
Here's what many people don't realize: you cannot determine whether a cutaneous horn is dangerous just by looking at it. The only way to know what's causing the horn is to remove it and examine it under a microscope.
Excisional Biopsy Process:
The pathologist will identify:
This information is essential for your long-term health and determines whether further treatment is needed.
The primary treatment for a cutaneous horn is complete surgical removal. Unlike some skin conditions that can be observed or treated with creams, cutaneous horns require excision for both diagnosis and treatment.
Even if a cutaneous horn appears benign, removal serves multiple important purposes:
✅ Diagnostic certainty – Determines the underlying cause
✅ Cancer screening – Rules out or identifies malignancy
✅ Prevents progression – Stops pre-cancerous lesions from advancing
✅ Symptom relief – Eliminates discomfort or cosmetic concerns
✅ Prevents trauma – Removes a projection that could be injured
Complete excisional removal is the recommended approach for nearly all cutaneous horns. This procedure:
The Procedure:
At The Minor Surgery Center, we specialize in these types of minor surgical procedures, providing expert care in a comfortable, efficient setting without long wait times.
In specific situations, other approaches may be considered:
Shave Excision For lesions with a very low suspicion of malignancy, a shave excision that removes the visible horn and superficial base may be performed. However, this provides less tissue for pathology and carries a higher recurrence risk.
Cryotherapy (Freezing) Liquid nitrogen can destroy some benign lesions, but this approach:
Electrosurgery Using electrical current to remove the lesion suffers from similar limitations as cryotherapy and is rarely the best choice.
Immediate Post-Procedure Care:
Pathology Results: Your provider will contact you once pathology results are available, typically within 1-2 weeks. Based on these findings:
You can learn more about what to expect from minor surgical procedures on our conditions page.
Understanding potential complications and long-term outlook helps you make informed decisions about treatment and follow-up care.
From the Lesion Itself:
From Treatment:
The outlook after cutaneous horn removal depends entirely on the underlying cause:
Benign Lesions:
Pre-Malignant Lesions (Actinic Keratosis, Bowen's Disease):
Malignant Lesions (Squamous Cell Carcinoma, Basal Cell Carcinoma):
Squamous Cell Carcinoma Specific Notes: When a cutaneous horn overlies squamous cell carcinoma, studies show:
"The key to the best outcome is early evaluation and complete removal. Don't wait—if you notice an unusual growth on your skin, have it checked promptly."
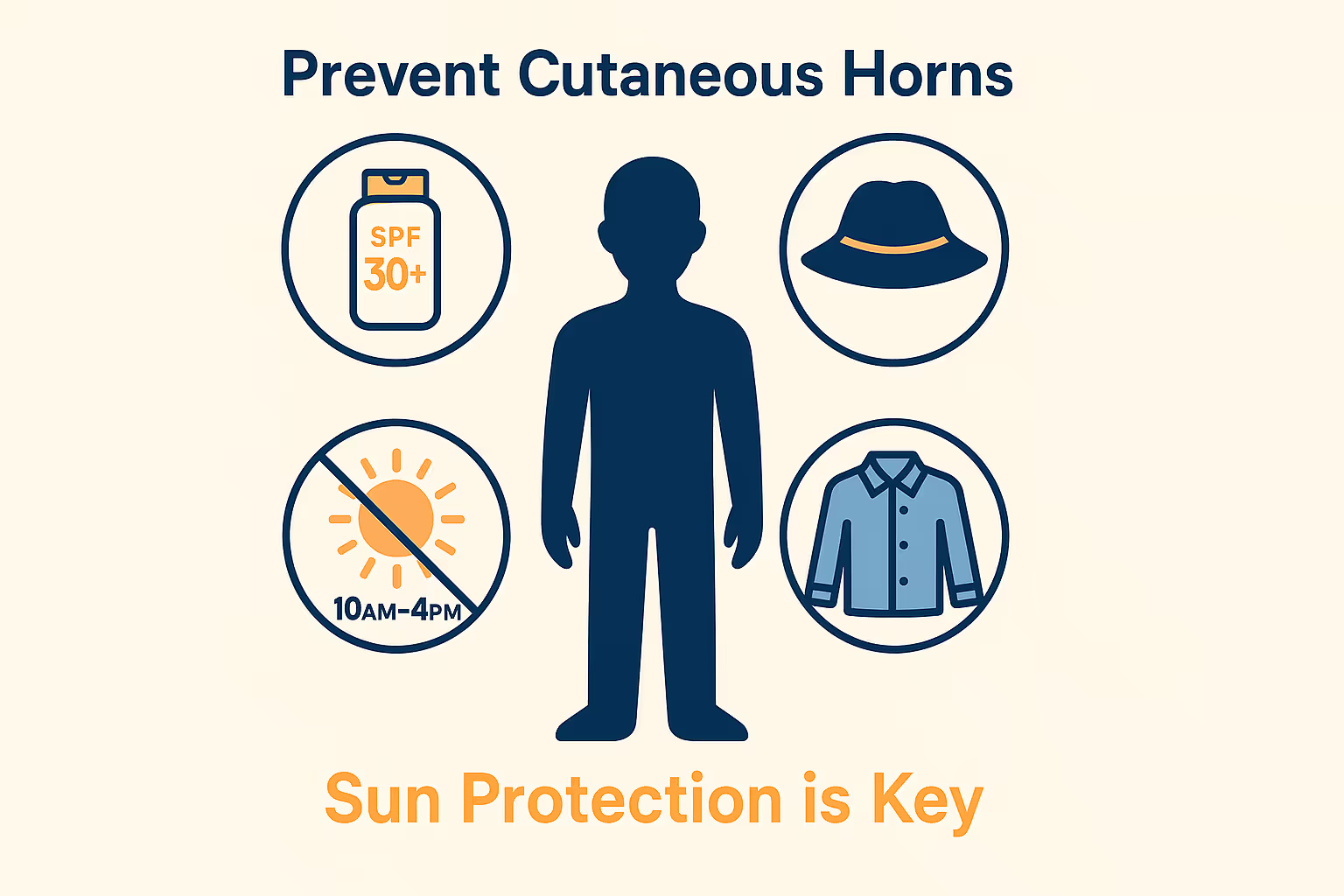
While you can't eliminate all risk, you can significantly reduce your chances of developing cutaneous horns and the underlying conditions that cause them.
Since UV radiation is the primary culprit behind most cutaneous horns, comprehensive sun protection is essential:
☀️ Daily Sunscreen
🧢 Protective Clothing
⏰ Timing Matters
🕶️ Eye and Lip Protection
Monthly skin checks help you detect changes early:
Annual skin checks by a healthcare provider are recommended for:
Our team at The Minor Surgery Center emphasizes prevention and early detection as cornerstones of skin health.
Knowing when to schedule an evaluation can make a significant difference in outcomes. Don't adopt a "wait and see" approach with unusual skin growths.
✓ Any new, horn-like growth on your skin
✓ A hard, protruding lesion that wasn't there before
✓ Changes in an existing skin lesion (size, color, shape, or texture)
✓ Bleeding, pain, or itching from a skin growth
✓ A lesion that won't heal or keeps recurring
✓ Any growth you're concerned about—trust your instincts
🚨 Rapid growth over days to weeks
🚨 Significant bleeding that doesn't stop with gentle pressure
🚨 Signs of infection (increasing pain, warmth, redness, pus)
🚨 A lesion on the genitals or other mucosal surfaces
🚨 Multiple lesions appearing simultaneously
When you visit a healthcare provider for evaluation:
At The Minor Surgery Center, we make this process straightforward and stress-free. No long wait times, no complicated referrals—just expert care when you need it.
Come prepared with questions to make the most of your appointment:
For more information about what to expect, visit our FAQs page.
Discovering you have a cutaneous horn can feel unsettling, but understanding what comes next empowers you to take control of your skin health.
It's completely normal to feel:
Remember: cutaneous horns are treatable, and most have benign or easily managed causes. The key is taking action rather than worrying in silence.
Before Removal:
Day of the Procedure:
Immediate Post-Procedure (First 24-48 Hours):
First Week:
Long-Term Healing:
After treatment for a cutaneous horn:
Self-Monitoring:
Professional Follow-Up:
Understanding the financial aspect of treatment helps with planning:
For an estimate of costs, check out our Minor Surgery Cost Estimator to get a better understanding of what to expect.
While very small horns occasionally break off due to trauma, this isn't a reliable or recommended approach. The underlying cause remains, and the horn will likely regrow. More importantly, you miss the opportunity for pathological examination to rule out cancer.
No, cutaneous horns themselves are not contagious. However, if the underlying cause is a viral wart (HPV), that virus can potentially spread to other areas of your body or to other people through direct contact.
Absolutely not. Home removal is dangerous and strongly discouraged because:
Always seek professional medical care for removal.
Growth rate varies considerably depending on the underlying cause. Some develop slowly over months to years, while others (particularly those overlying keratoacanthoma or aggressive cancers) can appear in just weeks. Any rapidly growing lesion deserves immediate medical attention.
Most insurance plans cover medically necessary removal of cutaneous horns, as the procedure is needed to diagnose the underlying condition and rule out cancer. Coverage for purely cosmetic concerns may vary. Contact your insurance provider or our office for specific information about your plan.
These are completely different lesions:
If the entire lesion including the base is completely removed with clear margins, recurrence is unlikely. However:
There are no safe or effective home remedies for cutaneous horns. Any growth that could potentially be cancerous requires professional medical evaluation and treatment. Attempting natural remedies delays diagnosis and could allow a cancer to progress.
When it comes to unusual skin growths like cutaneous horns, the expertise of your healthcare provider matters significantly. These lesions require careful evaluation, proper removal technique, and accurate pathological interpretation.
Experience Makes a Difference:
What to Look For in a Provider: ✓ Experience with skin lesion removal
✓ Access to pathology services
✓ Clear communication about the process
✓ Comfortable, professional environment
✓ Reasonable wait times for appointments
✓ Transparent pricing and billing
At The Minor Surgery Center, our experienced surgeons specialize in exactly these types of procedures. We combine medical expertise with a patient-focused approach that makes the process as comfortable and straightforward as possible.
We believe that expert medical care shouldn't come with long waits, confusing referrals, or unnecessary anxiety. Our process is designed to be:
Efficient: Quick appointment scheduling without months-long waits
Comprehensive: Thorough evaluation and complete removal with pathology
Comfortable: Modern facilities and compassionate care that puts you at ease
Transparent: Clear explanations, upfront pricing, and no surprises
Expert: Skilled surgeons with extensive experience in minor surgical procedures
You can learn more about our locations and services on our clinics page.
Cutaneous horns may look unusual, but they're a treatable condition that, when properly managed, rarely leads to serious complications. The key is understanding what you're dealing with and taking prompt action.
🔑 Don't ignore unusual skin growths. A cutaneous horn always deserves medical evaluation to determine the underlying cause.
🔑 Not all cutaneous horns are dangerous, but you can't tell by looking. Only pathological examination after removal provides a definitive answer.
🔑 Complete surgical removal is the gold standard treatment, serving both diagnostic and therapeutic purposes.
🔑 Sun protection is your best defense against the skin damage that leads to cutaneous horns and the conditions that cause them.
🔑 Early detection improves outcomes significantly, especially if the underlying cause is pre-cancerous or malignant.
If you've noticed a horn-like growth on your skin:
You deserve to feel comfortable and confident in your skin. That's why we make evaluation and removal of concerning skin growths fast, simple, and clear—without the wait.
Ready to take the next step? Visit The Minor Surgery Center to learn more about our services, find a location near you, or schedule a consultation. Our expert team is here to provide the professional care you need with the compassion you deserve.
Your skin health is too important to leave to chance. If you have a cutaneous horn or any concerning skin growth, reach out today. Early action leads to better outcomes, less worry, and peace of mind.
For more information about skin conditions we treat, visit our comprehensive blog with additional resources and expert insights.