Skin cancer affects millions of people worldwide, making it one of the most common forms of cancer today. Skin cancer spots can appear anywhere on the body, often disguising themselves as harmless moles or blemishes. Understanding how to identify these potentially dangerous lesions could literally save a life.
The human skin serves as the body's first line of defense against environmental threats, but prolonged exposure to ultraviolet radiation and other risk factors can cause normal skin cells to transform into cancerous ones. These transformed cells manifest as skin cancer spots that vary in appearance, size, and location depending on the type of cancer involved.
Early detection remains the most powerful weapon in the fight against skin cancer. When skin cancer spots are identified and treated in their initial stages, the survival rates are exceptionally high. However, delayed diagnosis can lead to serious complications, including metastasis to other parts of the body.
This comprehensive guide explores everything individuals need to know about skin cancer spots, from recognition and risk factors to treatment options and prevention strategies. Healthcare professionals emphasize that knowledge and vigilance are essential tools for protecting skin health and maintaining overall well-being.
• Skin cancer spots come in various forms, with melanoma, basal cell carcinoma, and squamous cell carcinoma being the three main types, each presenting distinct characteristics

• The ABCDE method (Asymmetry, Border, Color, Diameter, Evolving) provides a reliable framework for identifying suspicious skin cancer spots during self-examinations • Early detection dramatically improves treatment outcomes, with survival rates exceeding 95% when skin cancer spots are caught in their earliest stages • Regular professional skin examinations combined with monthly self-checks create the most effective strategy for monitoring skin cancer spots • Prevention through sun protection, including sunscreen use and protective clothing, remains the best defense against developing skin cancer spots
Skin cancer spots represent abnormal growths of skin cells that have undergone malignant transformation. These lesions develop when DNA damage accumulates in skin cells, typically due to ultraviolet radiation exposure from the sun or artificial sources like tanning beds. The damaged cells begin to multiply uncontrollably, forming visible growths on the skin's surface.
The appearance of skin cancer spots varies significantly depending on the type of cancer, location on the body, and stage of development. Some may appear as small, flesh-colored bumps, while others present as dark, irregularly shaped moles or red, scaly patches. Understanding these variations helps individuals recognize when professional medical evaluation becomes necessary.
Basal Cell Carcinoma (BCC) represents the most common form of skin cancer, accounting for approximately 80% of all cases. These skin cancer spots typically appear on sun-exposed areas such as the face, neck, and hands. BCC lesions often manifest as pearly or waxy bumps, flat flesh-colored or brown scar-like lesions, or bleeding or scabbing sores that heal and return.
Squamous Cell Carcinoma (SCC) ranks as the second most common type, comprising about 15% of skin cancer cases. These skin cancer spots frequently develop on areas with significant sun exposure, including the ears, face, neck, and hands. SCC lesions typically appear as firm red nodules, flat lesions with scaly or crusted surfaces, or new sores or raised areas on existing scars or ulcers.
Melanoma represents the most dangerous form of skin cancer, though it accounts for only about 5% of cases. These skin cancer spots can develop anywhere on the body, including areas with minimal sun exposure. Melanoma lesions often appear as new moles or changes in existing moles, with irregular shapes, multiple colors, and evolving characteristics.
Asymmetry serves as the first checkpoint when examining potential skin cancer spots. Normal moles typically display symmetrical shapes, meaning one half mirrors the other when divided by an imaginary line. Suspicious lesions often exhibit irregular, asymmetrical patterns where one portion differs significantly from the other.
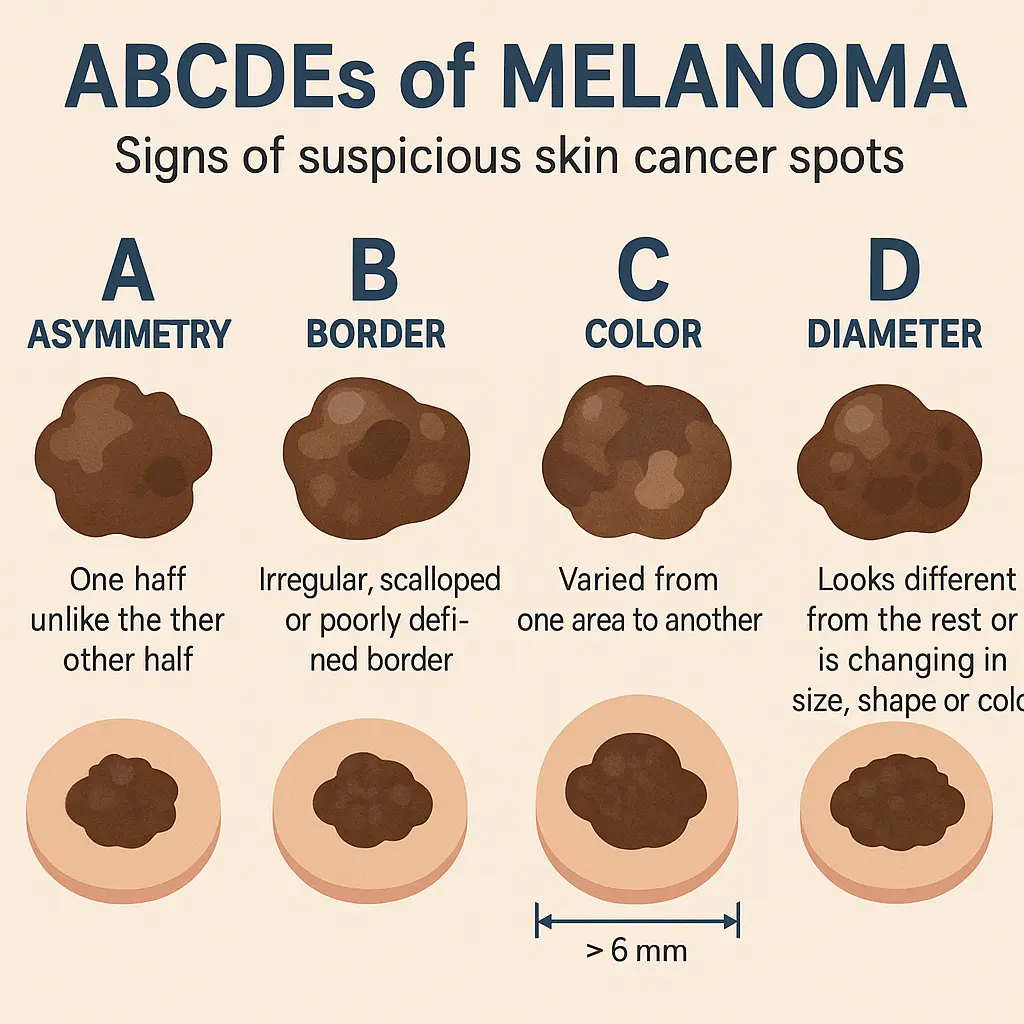
When conducting self-examinations, individuals should carefully observe each mole or spot, mentally dividing it in half both vertically and horizontally. Skin cancer spots, particularly melanomas, frequently display obvious asymmetry that becomes apparent during this simple assessment. Any mole showing clear asymmetrical characteristics warrants professional evaluation.
Border irregularities provide another crucial indicator of potentially malignant skin cancer spots. Benign moles typically maintain smooth, well-defined borders that create clear distinctions between the mole and surrounding skin. Cancerous lesions often develop irregular, notched, scalloped, or poorly defined borders.
The edges of suspicious skin cancer spots may appear blurred, jagged, or uneven, creating an unclear boundary between the lesion and normal skin. Some melanomas develop borders that seem to fade into the surrounding tissue, while others create sharp, irregular edges that change direction abruptly. These border characteristics often become more pronounced as the cancer progresses.
Color variations within a single lesion represent significant warning signs for skin cancer spots. Normal moles typically maintain uniform coloration throughout, usually appearing as consistent shades of brown, black, or flesh-colored. Malignant lesions often display multiple colors within the same spot, creating a variegated appearance.
Suspicious skin cancer spots may contain combinations of brown, black, red, white, or blue colors distributed unevenly throughout the lesion. Some melanomas develop areas of regression that appear white or flesh-colored, while other regions become darker or develop red inflammation. The presence of multiple colors within a single spot requires immediate professional assessment.
Diameter considerations help identify skin cancer spots that require closer attention. The general guideline suggests that lesions larger than 6 millimeters (about the size of a pencil eraser) deserve professional evaluation. However, melanomas can develop at smaller sizes, making this criterion just one component of comprehensive assessment.
Healthcare providers emphasize that skin cancer spots of any size showing other suspicious characteristics warrant examination, regardless of diameter. Some melanomas begin as small lesions that gradually increase in size, while others may remain relatively small but display concerning asymmetry, border irregularities, or color variations.
Evolution represents perhaps the most critical factor in identifying dangerous skin cancer spots. Any mole or lesion that changes in size, shape, color, elevation, or develops new symptoms like bleeding, itching, or crusting requires immediate attention. These evolutionary changes often signal malignant transformation.
Individuals should maintain awareness of their skin's normal appearance and note any modifications in existing skin cancer spots or the development of new lesions. Changes may occur gradually over months or years, or they may appear rapidly over weeks. Documentation through photography can help track these changes and provide valuable information for healthcare providers.
Professional medical evaluation becomes essential when skin cancer spots display any suspicious characteristics identified through self-examination. Individuals should schedule appointments with qualified healthcare providers when lesions show asymmetry, border irregularities, color variations, large diameter, or evolutionary changes. The Minor Surgery Center specializes in comprehensive skin cancer evaluation and treatment.
Additional warning signs that warrant immediate medical attention include skin cancer spots that bleed, itch, become tender, or develop crusting or scaling. New lesions that appear different from existing moles, particularly in individuals over age 30, also require professional assessment. Early intervention significantly improves treatment outcomes and reduces the risk of complications.
Healthcare providers employ various techniques to evaluate suspicious skin cancer spots during professional examinations. The process typically begins with a comprehensive visual inspection using specialized lighting and magnification tools called dermatoscopes. These instruments allow providers to examine skin structures not visible to the naked eye.
When skin cancer spots appear suspicious during visual examination, providers may recommend biopsy procedures to obtain tissue samples for laboratory analysis. Different biopsy techniques include shave biopsies, punch biopsies, and excisional biopsies, with the choice depending on the lesion's characteristics and location. The conditions treated at specialized centers include comprehensive skin cancer diagnosis and management.
Modern dermatology utilizes sophisticated technologies to enhance the accuracy of skin cancer spots diagnosis. Digital dermoscopy creates high-resolution images that can be compared over time to detect subtle changes in lesions. Some facilities employ artificial intelligence systems that analyze dermoscopic images and provide additional diagnostic insights.
Confocal microscopy represents another advanced technique that allows real-time visualization of skin cancer spots at the cellular level without requiring tissue removal. This technology helps providers distinguish between benign and malignant lesions with greater precision, potentially reducing the need for unnecessary biopsies while ensuring appropriate treatment for cancerous lesions.
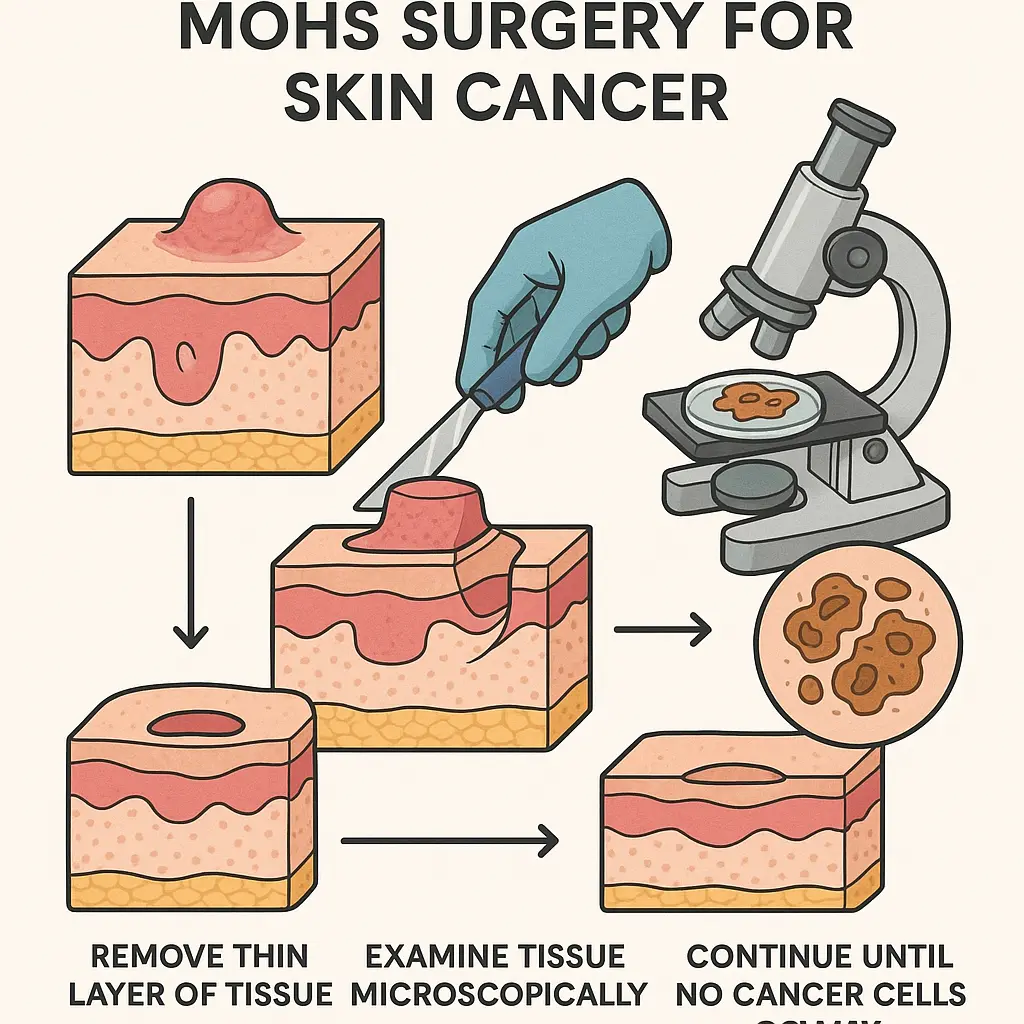
Surgical removal remains the primary treatment for most skin cancer spots, with various techniques available depending on the cancer type, size, and location. Simple excision involves removing the lesion along with a margin of healthy tissue to ensure complete elimination of cancerous cells. This approach works well for smaller lesions with well-defined borders.

Mohs surgery represents the gold standard for treating certain skin cancer spots, particularly those in cosmetically sensitive areas or with high recurrence risks. This technique involves removing thin layers of tissue and examining them microscopically until no cancer cells remain. The team of specialists provides expert surgical care for various skin cancer types.
Topical therapies offer alternatives for specific types of skin cancer spots, particularly superficial basal cell carcinomas and certain precancerous lesions. Medications like imiquimod stimulate the immune system to attack cancer cells, while 5-fluorouracil directly targets rapidly dividing cells. These treatments require several weeks of application and regular monitoring.
Cryotherapy uses liquid nitrogen to freeze and destroy skin cancer spots, making it suitable for small, superficial lesions. The procedure involves applying extreme cold to the affected area, causing cancer cells to die and eventually slough off. Multiple treatment sessions may be necessary for complete elimination of the lesion.
Radiation therapy provides an option for skin cancer spots in locations where surgery might be challenging or for patients who cannot undergo surgical procedures. External beam radiation delivers targeted energy to destroy cancer cells while minimizing damage to surrounding healthy tissue. Treatment typically involves multiple sessions over several weeks.
Photodynamic therapy combines light-sensitive medications with specific wavelengths of light to destroy skin cancer spots. This approach works particularly well for superficial lesions and can treat multiple areas simultaneously. The treatment involves applying a photosensitizing agent followed by light exposure after an appropriate waiting period.
Sunscreen application forms the cornerstone of skin cancer spots prevention, requiring broad-spectrum protection with SPF 30 or higher. Proper application involves using approximately one ounce of sunscreen for the entire body, applying it 15-30 minutes before sun exposure, and reapplying every two hours or after swimming or sweating.
Protective clothing provides physical barriers against ultraviolet radiation that can lead to skin cancer spots. Long-sleeved shirts, wide-brimmed hats, and sunglasses with UV protection significantly reduce exposure to harmful rays. Specially designed UV-protective clothing offers additional benefits for individuals spending extended periods outdoors.
Seeking shade during peak UV hours between 10 AM and 4 PM dramatically reduces the risk of developing skin cancer spots. When outdoor activities are necessary during these times, individuals should prioritize shaded areas and limit direct sun exposure. Even on cloudy days, UV radiation can penetrate clouds and cause skin damage.
Avoiding tanning beds eliminates a significant risk factor for skin cancer spots, as artificial UV radiation can be more intense than natural sunlight. The World Health Organization classifies tanning bed use as a Group 1 carcinogen, placing it in the same category as tobacco and asbestos. Natural tanning also increases cancer risk and should be minimized.
Monthly self-examinations enable early detection of skin cancer spots by helping individuals become familiar with their skin's normal appearance. These examinations should include all body areas, using mirrors to check difficult-to-see locations like the back and scalp. Any new or changing lesions should prompt professional evaluation.
Professional skin examinations complement self-checks by providing expert assessment of potential skin cancer spots. Dermatologists recommend annual screenings for most adults, with more frequent examinations for high-risk individuals. These appointments allow for professional documentation of existing moles and identification of suspicious changes. For comprehensive evaluation, patients can visit the clinic for expert assessment.
Fair skin complexion significantly increases the risk of developing skin cancer spots due to lower levels of protective melanin pigment. Individuals with light hair, blue or green eyes, and skin that burns easily face elevated risks and require enhanced protection measures. However, skin cancer can affect people of all skin types and ethnicities.
Family history of skin cancer creates genetic predisposition to developing skin cancer spots, making regular monitoring essential for affected individuals. Certain genetic conditions like xeroderma pigmentosum dramatically increase cancer risk by impairing the body's ability to repair UV-induced DNA damage. These individuals require extreme sun protection measures.
Geographic location influences skin cancer spots risk, with higher rates occurring in areas closer to the equator where UV radiation is more intense. Altitude also affects exposure levels, as UV radiation increases approximately 4% for every 1,000 feet of elevation. Individuals living in or visiting high-risk areas should take additional precautions.
Occupational exposure affects certain professions where workers spend significant time outdoors, increasing their risk of developing skin cancer spots. Construction workers, farmers, lifeguards, and outdoor sports professionals face elevated risks and should implement comprehensive protection strategies including protective clothing, sunscreen, and regular skin monitoring.
Previous skin cancer diagnosis substantially increases the risk of developing additional skin cancer spots, making ongoing surveillance crucial for affected individuals. Studies show that people with a history of one skin cancer have a significantly higher likelihood of developing subsequent lesions, requiring lifetime monitoring and protection.
Immunosuppression from medical conditions or medications increases vulnerability to skin cancer spots by reducing the body's ability to identify and eliminate abnormal cells. Organ transplant recipients, individuals with certain autoimmune conditions, and those taking immunosuppressive medications require enhanced monitoring and protection strategies.
Regular surveillance becomes essential after treatment of skin cancer spots to monitor for recurrence and detect new lesions early. Follow-up schedules vary based on cancer type, stage, and individual risk factors, but typically include examinations every 3-6 months initially, extending to annual visits for low-risk cases. These appointments allow healthcare providers to assess healing and identify any concerning changes.
Scar management following surgical removal of skin cancer spots involves proper wound care and sun protection of treated areas. Surgical scars remain more susceptible to UV damage and require diligent sunscreen application. Some patients benefit from scar treatment options to improve cosmetic outcomes while maintaining cancer surveillance.
Anxiety management addresses the emotional impact of skin cancer spots diagnosis and treatment, as many patients experience ongoing concerns about recurrence or developing new lesions. Support groups, counseling services, and educational resources help individuals cope with these challenges while maintaining appropriate vigilance without excessive worry.
Quality of life considerations focus on helping patients return to normal activities while incorporating necessary protection measures. This balance involves maintaining outdoor recreational activities with proper sun protection, addressing cosmetic concerns from treatment, and developing sustainable long-term monitoring routines.
Many individuals wonder about the appropriate frequency for checking skin cancer spots and scheduling professional examinations. Monthly self-examinations provide optimal balance between vigilance and practicality, allowing individuals to become familiar with their skin's normal appearance while detecting changes promptly. Professional examinations should occur annually for most adults, with more frequent visits for high-risk individuals.
The timing of skin cancer spots examinations should consider seasonal factors, as many people notice changes after summer sun exposure. Scheduling professional visits in early fall allows assessment of any summer-related changes while providing time to address concerning lesions before winter months when healing may be optimal.
Biopsy interpretation for skin cancer spots involves understanding various diagnostic terms that pathologists use to describe tissue samples. Benign results indicate no cancer cells present, while malignant results confirm cancer diagnosis and provide specific information about cancer type and characteristics. Some results may indicate atypical or dysplastic changes that require monitoring or additional treatment.
Staging information helps patients understand the extent of skin cancer spots and treatment implications. Early-stage cancers confined to the skin surface have excellent prognosis with simple treatments, while advanced stages may require more extensive intervention. Understanding these classifications helps patients make informed decisions about treatment options. For detailed information about various conditions and treatments, patients can explore the frequently asked questions section.
Artificial intelligence applications are revolutionizing skin cancer spots detection by analyzing images with accuracy levels matching or exceeding dermatologists in some studies. These technologies may eventually enable smartphone-based screening tools that help individuals identify suspicious lesions before professional examination, though they cannot replace expert medical evaluation.
Liquid biopsy techniques represent promising developments for monitoring skin cancer spots recurrence and treatment response. These blood tests can detect circulating tumor cells or DNA fragments, potentially identifying cancer recurrence before visible lesions appear. While still in development, these technologies may transform follow-up care protocols.
Immunotherapy advances offer new hope for treating advanced skin cancer spots, particularly melanoma cases that have spread beyond the original site. These treatments harness the body's immune system to fight cancer cells more effectively than traditional chemotherapy, often with fewer side effects and improved outcomes.
Targeted therapy approaches focus on specific genetic mutations found in certain skin cancer spots, allowing for personalized treatment strategies. These medications target particular pathways that cancer cells use for growth and survival, offering more precise treatment with potentially better results and reduced side effects.
Understanding skin cancer spots empowers individuals to take proactive steps in protecting their skin health and detecting potential problems early. The knowledge gained from recognizing warning signs, understanding risk factors, and implementing prevention strategies creates a foundation for lifelong skin cancer vigilance.
Regular self-examinations combined with professional screenings provide the most effective strategy for early detection of skin cancer spots. This dual approach ensures that both obvious and subtle changes receive appropriate attention, maximizing the chances of successful treatment outcomes when cancer does occur.
Prevention remains paramount in reducing the risk of developing skin cancer spots through consistent sun protection measures, lifestyle modifications, and awareness of personal risk factors. These strategies, when implemented consistently, can significantly reduce cancer risk while allowing individuals to maintain active, outdoor lifestyles safely.
The importance of professional medical evaluation cannot be overstated when suspicious skin cancer spots are identified. Healthcare providers possess the expertise, tools, and experience necessary to accurately diagnose and treat skin cancer effectively. Early intervention saves lives and often allows for simpler, less invasive treatments with better cosmetic outcomes.
For individuals concerned about skin cancer spots or seeking professional evaluation, contacting qualified healthcare providers represents the most important step in ensuring optimal outcomes. The contact information for specialized care facilities provides access to expert evaluation and treatment services.
Remember that skin cancer spots detection and treatment have never been more effective than today, with survival rates exceeding 95% when cancer is caught early. This encouraging statistic reinforces the value of vigilance, education, and prompt action when concerning lesions are identified. Taking control of skin health through knowledge and appropriate medical care provides the best protection against this common but highly treatable form of cancer.
The journey of skin cancer awareness begins with education and continues with consistent application of protection and monitoring strategies. By understanding skin cancer spots and taking appropriate action, individuals can maintain healthy skin while enjoying life's outdoor activities safely and confidently.