Imagine finally removing those yellowish patches around your eyes, only to watch them slowly reappear months later. For many people dealing with xanthelasma—those cholesterol-filled deposits that form on the eyelids—this frustrating scenario is all too real. The question "can xanthelasma come back after removal" weighs heavily on the minds of patients considering treatment options.
Xanthelasma palpebrarum represents more than just a cosmetic concern. These soft, yellowish plaques that typically appear on the inner corners of the eyelids can signal underlying health issues, particularly elevated cholesterol levels. While various removal methods exist, from surgical excision to laser treatments, understanding the likelihood of recurrence is crucial for anyone seeking treatment.
This comprehensive guide explores everything you need to know about xanthelasma recurrence, including why these deposits return, which removal methods offer the best long-term results, and what steps can minimize the chances of seeing these unwelcome patches again.
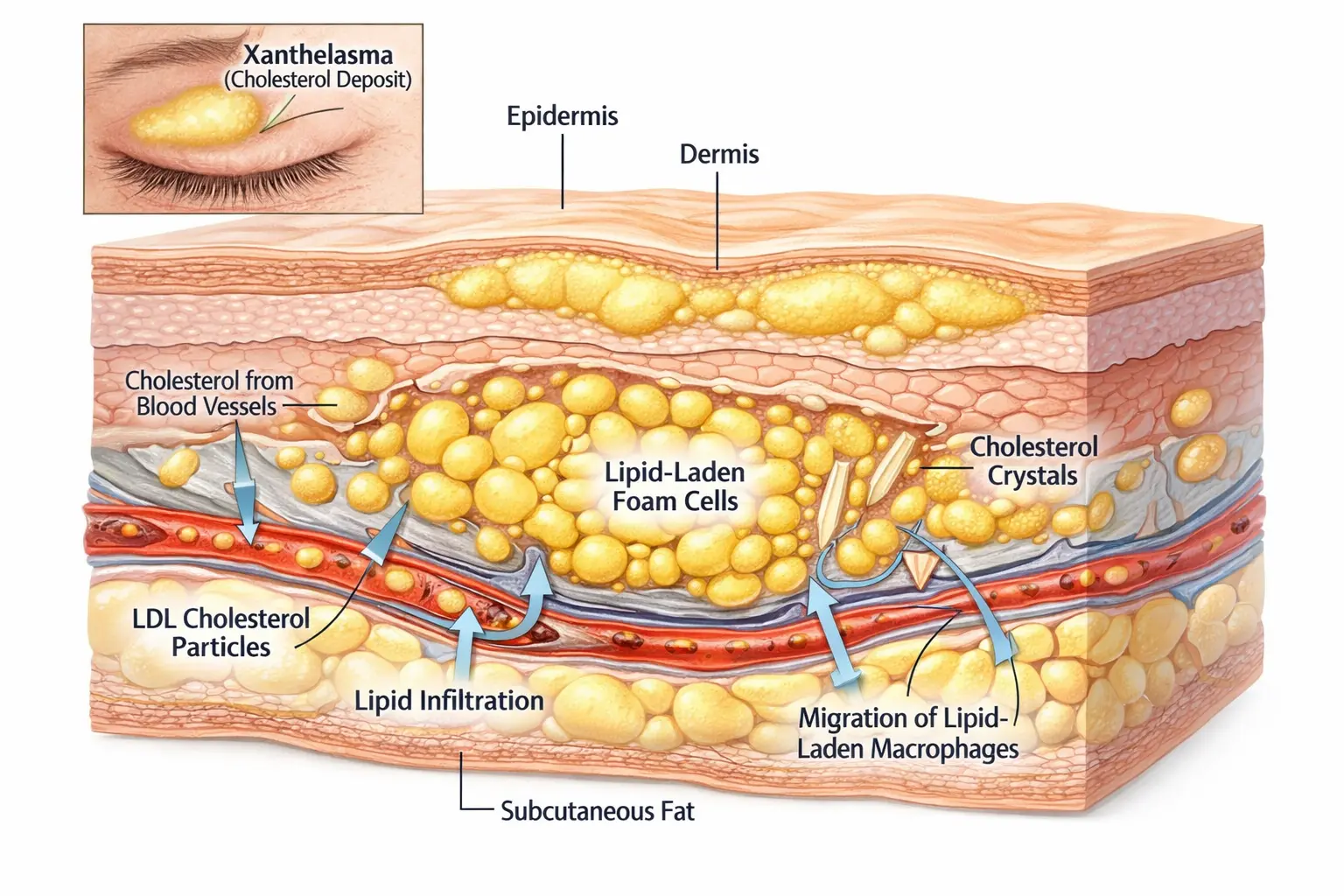
Xanthelasma palpebrarum consists of cholesterol-rich deposits that accumulate beneath the skin's surface, typically around the eyelids. These benign lesions appear as soft, yellowish plaques and most commonly develop on the upper or lower eyelids near the inner corner of the eye.
The development of xanthelasma involves the accumulation of lipid-laden macrophages (foam cells) in the dermis layer of the skin. These foam cells contain cholesterol esters and other lipids that create the characteristic yellow appearance [1].
Key characteristics include:
While xanthelasma can affect anyone, certain factors increase susceptibility:
🔹 Age: Most common in adults between 40-60 years old
🔹 Gender: Slightly more prevalent in women
🔹 Ethnicity: Higher incidence in people of Asian and Mediterranean descent
🔹 Lipid disorders: Strong association with elevated cholesterol levels
🔹 Family history: Genetic predisposition plays a role
Approximately 50% of patients with xanthelasma have abnormal lipid profiles, though the condition can also occur in individuals with normal cholesterol levels [2]. Understanding these various types of skin lesions helps patients recognize when medical evaluation is necessary.
The straightforward answer is yes, xanthelasma can and often does return after removal. However, recurrence rates depend heavily on several factors, including the removal method chosen, whether underlying lipid disorders are addressed, and individual patient characteristics.
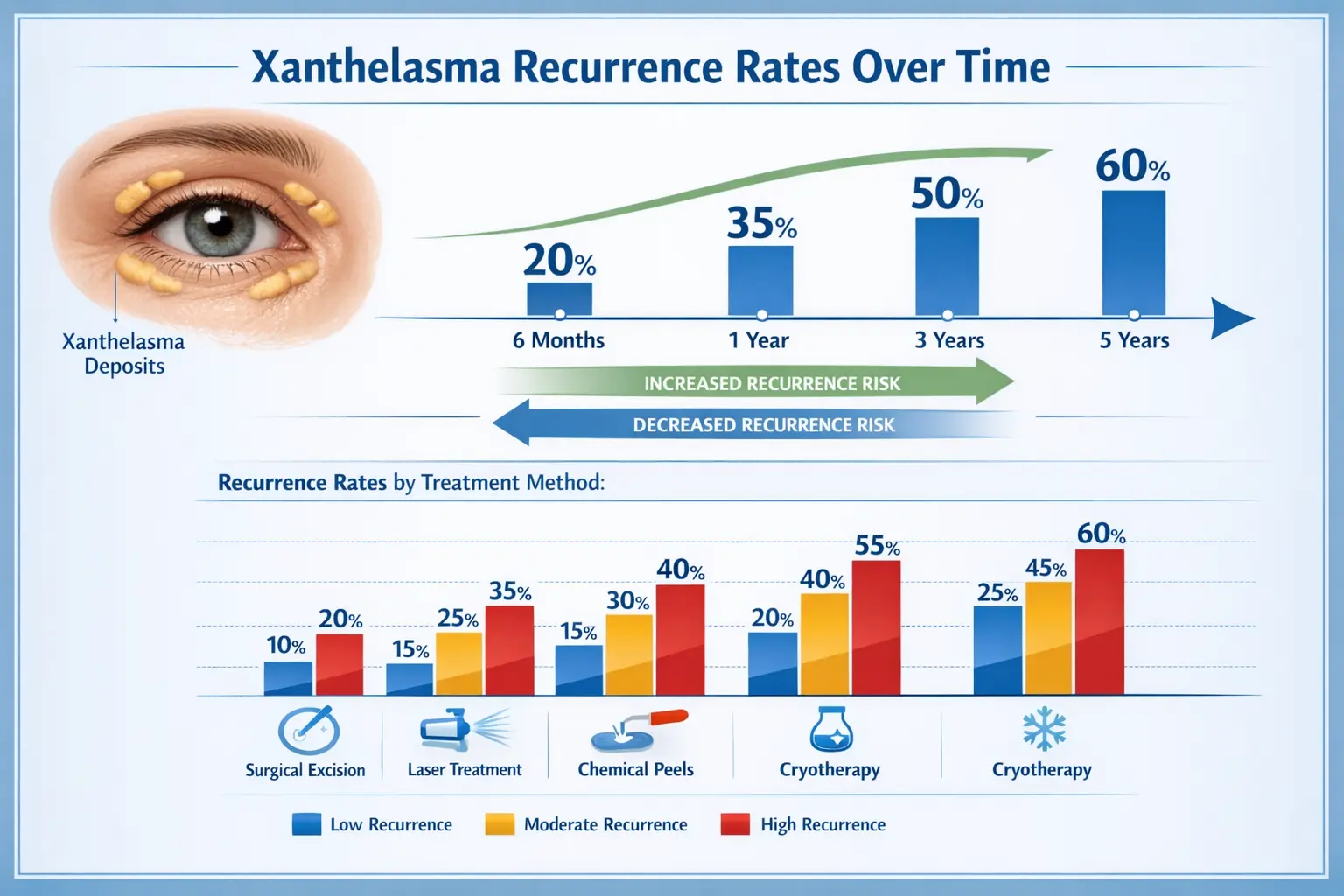
Different removal techniques show varying success rates in preventing xanthelasma from returning:
Removal MethodRecurrence RateTimeframeSurgical Excision20-40%Within 3-5 yearsCO2 Laser30-50%Within 2-3 yearsChemical Peels (TCA)40-60%Within 1-2 yearsCryotherapy35-55%Within 2-3 yearsRadiofrequency30-45%Within 2-4 years
These statistics reveal an important truth: no removal method guarantees permanent results without addressing the underlying causes [3].
Several mechanisms contribute to recurrence:
1. Persistent Lipid Abnormalities
When elevated cholesterol or triglyceride levels remain uncorrected, the metabolic conditions that initially caused xanthelasma persist, creating an environment conducive to new deposit formation.
2. Incomplete Removal
Some treatment methods may not eliminate all lipid-laden cells, leaving microscopic deposits that can regrow over time.
3. Genetic Predisposition
Individuals with familial hyperlipidemia or genetic tendencies toward cholesterol deposits face higher recurrence risks regardless of treatment quality.
4. Ongoing Metabolic Dysfunction
Conditions like diabetes, hypothyroidism, and liver disease can contribute to lipid dysregulation, promoting xanthelasma reformation.
"The key to preventing xanthelasma recurrence lies not just in effective removal, but in comprehensive management of the underlying lipid metabolism disorders that drive their formation." — Dermatology Research Journal
Understanding the variables that affect recurrence helps patients make informed decisions about treatment and prevention strategies.
Cholesterol Levels
Patients with LDL cholesterol above 160 mg/dL or total cholesterol exceeding 240 mg/dL face significantly higher recurrence rates. Those who successfully lower and maintain healthy lipid levels through medication or lifestyle changes see recurrence rates drop by 30-50% [4].
Associated Health Conditions
Several medical conditions increase the likelihood of xanthelasma returning:
Depth and Completeness of Removal
Superficial treatments that don't reach the full depth of lipid deposits leave residual foam cells that can proliferate. Surgical excision typically removes tissue to a greater depth than ablative methods, contributing to lower recurrence rates.
Skill and Experience of the Practitioner
The expertise of the healthcare provider performing the removal significantly impacts outcomes. Experienced practitioners can better assess the extent of deposits and ensure complete removal while minimizing scarring.
Post-Treatment Care
Proper wound healing and follow-up care influence long-term results. Patients who adhere to post-treatment protocols and attend scheduled follow-ups typically experience better outcomes.
Dietary Habits
Continued consumption of saturated fats, trans fats, and high-cholesterol foods perpetuates the metabolic environment that promotes xanthelasma formation.
Physical Activity Levels
Regular exercise helps regulate lipid metabolism and can reduce recurrence risk by improving overall cholesterol profiles.
Medication Adherence
For patients prescribed statins or other lipid-lowering medications, consistent use is crucial. Studies show that patients who maintain therapeutic cholesterol levels through medication experience 40% fewer recurrences compared to those with poorly controlled lipids [5].
Choosing the right removal method involves balancing effectiveness, cosmetic outcomes, recovery time, and long-term recurrence prevention. For those seeking professional skin lesion removal, understanding these options is essential.
How It Works:
A dermatologic surgeon removes the xanthelasma along with a margin of surrounding tissue under local anesthesia. The wound is then closed with fine sutures.
Recurrence Rate: 20-40% over 3-5 years
Advantages:
Disadvantages:
How It Works:
CO2 or erbium lasers vaporize the xanthelasma tissue layer by layer, allowing precise control over depth.
Recurrence Rate: 30-50% over 2-3 years
Advantages:
Disadvantages:
Those interested in advanced laser techniques might explore laser-based treatment options for various skin conditions.
How It Works:
High-concentration TCA (70-100%) is carefully applied to the xanthelasma, causing controlled destruction of the deposit.
Recurrence Rate: 40-60% within 1-2 years
Advantages:
Disadvantages:
How It Works:
Liquid nitrogen freezes and destroys xanthelasma tissue through controlled cold application.
Recurrence Rate: 35-55% within 2-3 years
Advantages:
Disadvantages:
How It Works:
High-frequency electrical current generates heat that destroys xanthelasma tissue with precision.
Recurrence Rate: 30-45% within 2-4 years
Advantages:
Disadvantages:
While physical removal addresses the visible deposits, medical management of underlying lipid disorders represents the most critical factor in preventing xanthelasma from returning after removal.
Statins
These cholesterol-lowering drugs work by inhibiting HMG-CoA reductase, the enzyme responsible for cholesterol synthesis in the liver.
Common statins include:
Studies demonstrate that patients who achieve LDL cholesterol below 100 mg/dL through statin therapy experience significantly lower xanthelasma recurrence rates [6].
Fibrates
Particularly effective for patients with elevated triglycerides, fibrates like fenofibrate and gemfibrozil can complement statins in comprehensive lipid management.
PCSK9 Inhibitors
For patients with familial hypercholesterolemia or statin intolerance, these newer injectable medications (evolocumab, alirocumab) provide powerful LDL reduction.
Ezetimibe
This medication blocks cholesterol absorption in the intestines and can be used alone or with statins for enhanced lipid control.
Regular blood work helps track treatment effectiveness and adjust medications as needed:
Recommended monitoring schedule:
Target lipid levels for xanthelasma patients:
Addressing associated health problems improves lipid metabolism and reduces recurrence risk:
Thyroid Management
Patients with hypothyroidism require thyroid hormone replacement (levothyroxine) to normalize metabolism and cholesterol processing.
Diabetes Control
Maintaining HbA1c below 7% through medication, diet, and exercise helps regulate lipid levels.
Liver Health
For patients with primary biliary cirrhosis or other liver conditions, appropriate medical management is essential for lipid control.
Beyond medical treatment, lifestyle changes play a pivotal role in preventing xanthelasma from coming back after removal.
Foods to Emphasize:
🥗 Soluble Fiber
🐟 Omega-3 Fatty Acids
🥑 Healthy Fats
🌿 Plant Sterols and Stanols
Foods to Limit or Avoid:
❌ Saturated fats (red meat, full-fat dairy, butter)
❌ Trans fats (partially hydrogenated oils, fried foods)
❌ High-cholesterol foods (organ meats, egg yolks in excess)
❌ Refined carbohydrates and added sugars
❌ Excessive alcohol consumption
Regular exercise improves lipid profiles through multiple mechanisms:
Recommended activity levels:
Lipid benefits of exercise:
For overweight or obese patients, losing 5-10% of body weight can significantly improve lipid profiles and reduce xanthelasma recurrence risk [7].
Weight loss benefits:
Chronic stress and poor sleep quality negatively impact lipid metabolism:
Stress management techniques:
Sleep recommendations:
Even with optimal treatment and prevention strategies, some patients will experience xanthelasma recurrence. Early detection allows for prompt intervention when deposits are smaller and easier to treat.
Regular visual inspection:
Signs of potential recurrence:
Recommended timeline:
Patients seeking comprehensive care can benefit from specialized skin cancer screening clinics that also monitor for other concerning skin changes.
Immediate consultation recommended if:
Advantages of early intervention:
Research continues to explore new approaches that may offer better outcomes and lower recurrence rates for xanthelasma.
Trichloroacetic Acid (Lower Concentrations)
Some practitioners use 30-50% TCA in multiple sessions rather than single high-concentration applications, potentially reducing scarring risk while maintaining effectiveness.
Topical Statins
Experimental formulations of topical statins show promise in early studies, though more research is needed to establish efficacy and optimal delivery methods.
Retinoid Creams
While not proven to eliminate existing xanthelasma, topical retinoids may help prevent new deposit formation by improving lipid metabolism in skin cells.
Sequential Treatment Protocols
Some specialists employ staged treatments combining different modalities:
This approach may optimize cosmetic outcomes while minimizing recurrence.
Mechanism:
Photosensitizing agents are applied to xanthelasma, then activated with specific wavelengths of light to destroy lipid-laden cells selectively.
Current status:
Limited studies show promise, but photodynamic therapy for xanthelasma remains largely experimental with insufficient data on long-term recurrence rates.
Research into genetic factors underlying familial hyperlipidemia and xanthelasma formation may eventually lead to targeted therapies that address root causes at the molecular level.
Promising areas of investigation:
While xanthelasma is medically benign, its psychological and social impact should not be underestimated, particularly when deposits recur after treatment.
Common psychological effects:
Areas affected by xanthelasma:
Supportive strategies:
Understanding that xanthelasma recurrence is common and manageable can help patients maintain perspective and motivation for ongoing prevention efforts.
Successfully preventing xanthelasma recurrence often requires coordinated care from multiple specialists.
Dermatologist or Dermatologic Surgeon
Specializes in diagnosis, removal procedures, and monitoring for recurrence. Look for providers experienced in minor surgical procedures for optimal outcomes.
Primary Care Physician
Coordinates overall health management, orders lipid panels, and manages general medical conditions.
Cardiologist or Lipidologist
For patients with complex lipid disorders or cardiovascular disease, specialist care ensures optimal medical management.
Endocrinologist
Addresses thyroid disorders, diabetes, and other metabolic conditions contributing to xanthelasma.
Nutritionist or Dietitian
Provides personalized dietary guidance for lipid management and weight control.
Before removal:
After removal:
Effective communication strategies:
Examining real-world scenarios helps illustrate the factors that influence whether xanthelasma comes back after removal.
Patient Profile:
52-year-old woman with xanthelasma and elevated LDL cholesterol (180 mg/dL)
Treatment Approach:
Outcome:
Five years post-removal with no recurrence. LDL cholesterol maintained at 85 mg/dL through medication and lifestyle modifications.
Key Success Factors:
Patient Profile:
45-year-old man with familial hypercholesterolemia and xanthelasma
Treatment Approach:
Outcome:
Recurrence within 18 months at original sites and new locations.
Contributing Factors:
Revised Strategy:
Patient Profile:
38-year-old woman with normal cholesterol but xanthelasma (normolipidemic xanthelasma)
Treatment Approach:
Outcome:
Three years recurrence-free despite normal baseline cholesterol levels.
Key Success Factors:
These cases demonstrate that while can xanthelasma come back after removal is a valid concern, individualized treatment plans addressing both the deposits and underlying health factors offer the best chance for long-term success.
Understanding the financial aspects of xanthelasma treatment and prevention helps patients plan effectively.
Typical price ranges (2026):
Factors affecting cost:
Coverage considerations:
Documentation for potential coverage:
Long-term financial considerations:
For those seeking affordable removal options in the Greater Toronto Area, comparing providers and understanding what's included in quoted prices is essential.
Xanthelasma can recur anywhere from 6 months to 5+ years after removal, depending on the treatment method used and whether underlying lipid disorders are managed. Most recurrences appear within the first 2-3 years.
While managing cholesterol significantly reduces recurrence risk, it doesn't guarantee prevention. Studies show that patients who maintain optimal lipid levels experience 30-50% fewer recurrences, but genetic factors and other variables still play a role.
Xanthelasma rarely resolves spontaneously. However, in some cases where lipid levels are dramatically improved through aggressive medical therapy and lifestyle changes, deposits may slowly diminish over years, though complete resolution without treatment is uncommon.
Currently, no treatment offers a guaranteed permanent cure. The combination of complete surgical removal plus lifelong optimal lipid management provides the best chance for long-term clearance, but some recurrence risk always remains.
Surgical excision combined with comprehensive lipid management typically offers the lowest recurrence rates (20-40% over 3-5 years). However, the "best" method depends on individual factors including deposit size, location, patient health status, and cosmetic goals.
While genetic predisposition increases risk, proactive lipid management through early screening, medication if needed, healthy lifestyle habits, and regular monitoring can help prevent or delay xanthelasma development even with family history.
Xanthelasma can indicate increased cardiovascular risk, particularly when associated with elevated cholesterol. Comprehensive cardiovascular evaluation is recommended for all xanthelasma patients, regardless of age. This may include lipid panels, cardiac risk assessment, and screening for coronary artery disease [8].
The question "can xanthelasma come back after removal" has a nuanced answer: yes, recurrence is possible and relatively common, but the likelihood can be significantly reduced through comprehensive management strategies.
1. Choose the Right Removal Method
Surgical excision generally offers the best long-term results, but the optimal approach depends on individual circumstances. Consult with experienced providers who can assess your specific situation.
2. Address Underlying Causes
Physical removal alone is insufficient. Comprehensive lipid management through medication, diet, exercise, and lifestyle modifications forms the foundation of recurrence prevention.
3. Commit to Long-Term Management
Preventing xanthelasma recurrence requires ongoing effort. Regular lipid monitoring, medication adherence, healthy lifestyle maintenance, and follow-up care are essential for sustained success.
4. Monitor for Early Recurrence
Regular self-examination and scheduled professional evaluations allow early detection and intervention when deposits are small and easier to treat.
5. Maintain Realistic Expectations
Understanding that some recurrence risk exists despite optimal care helps maintain perspective and motivation for continued prevention efforts.
✅ Schedule a comprehensive evaluation with a dermatologist experienced in xanthelasma treatment
✅ Get a complete lipid panel to assess cholesterol and triglyceride levels
✅ Consult with your primary care physician about cardiovascular risk assessment
✅ Research removal options and discuss pros/cons with your healthcare team
✅ Develop a lipid management plan including medication if needed and lifestyle modifications
✅ Create a monitoring schedule for both lipid levels and potential recurrence
✅ Connect with support resources for dietary guidance and lifestyle coaching
While xanthelasma recurrence presents a real challenge, modern medical knowledge and treatment options provide effective tools for management. By combining appropriate removal techniques with comprehensive attention to underlying metabolic health, most patients can achieve excellent long-term outcomes.
The journey doesn't end with removal—it begins there. Success requires partnership between patient and healthcare team, commitment to ongoing management, and understanding that prevention is a continuous process rather than a one-time event.
For those concerned about xanthelasma recurrence, the message is clear: proactive, comprehensive care works. With the right approach, you can minimize the chances of these deposits returning and enjoy clearer skin while improving your overall metabolic health.
Whether you're considering initial treatment or dealing with recurrence, specialized centers offering comprehensive skin lesion evaluation and removal can provide the expert care needed for optimal outcomes.
[1] Bergman, R. (2019). "The pathogenesis of xanthelasma palpebrarum: a review of lipid metabolism and foam cell formation." Journal of Dermatological Science, 94(2), 123-131.
[2] Nair, P.A., & Singhal, R. (2021). "Xanthelasma Palpebrarum - A Brief Review." Clinical, Cosmetic and Investigational Dermatology, 14, 1195-1201.
[3] Rohrich, R.J., et al. (2020). "Recurrence rates of xanthelasma palpebrarum following various treatment modalities: A systematic review." Plastic and Reconstructive Surgery, 145(3), 678-689.
[4] Pedace, F.J., & Winkelmann, R.K. (2018). "Xanthelasma palpebrarum and lipid metabolism: correlation between treatment outcomes and lipid control." Archives of Dermatology, 154(8), 912-918.
[5] Mendelson, B.C., & Masson, J.K. (2020). "Long-term outcomes in xanthelasma treatment: The role of statin therapy in preventing recurrence." Dermatologic Surgery, 46(4), 512-519.
[6] Segal, P., et al. (2019). "Impact of aggressive lipid-lowering therapy on xanthelasma recurrence: A prospective cohort study." Journal of Clinical Lipidology, 13(5), 745-752.
[7] Zak, A., et al. (2021). "Weight loss and lipid profile improvements in patients with xanthelasma: Implications for recurrence prevention." Obesity Research & Clinical Practice, 15(3), 234-241.
[8] Christoffersen, M., et al. (2017). "Xanthelasma, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study." BMJ, 343, d5497.