Picture a young teenage boy suddenly experiencing frequent nosebleeds that won't stop, combined with difficulty breathing through his nose. What might seem like common adolescent issues could actually signal the presence of angiofibroma—a rare but significant vascular tumor that demands immediate medical attention. While these growths are non-cancerous, their aggressive local behavior and tendency to recur make them one of the most challenging conditions dermatologists and ENT specialists encounter.

Angiofibroma represents a group of benign vascular tumors that can develop in various parts of the body, with the most clinically significant variant being juvenile nasopharyngeal angiofibroma (JNA). Despite their non-cancerous nature, these tumors exhibit remarkably aggressive local behavior that can create serious complications if left untreated [1].
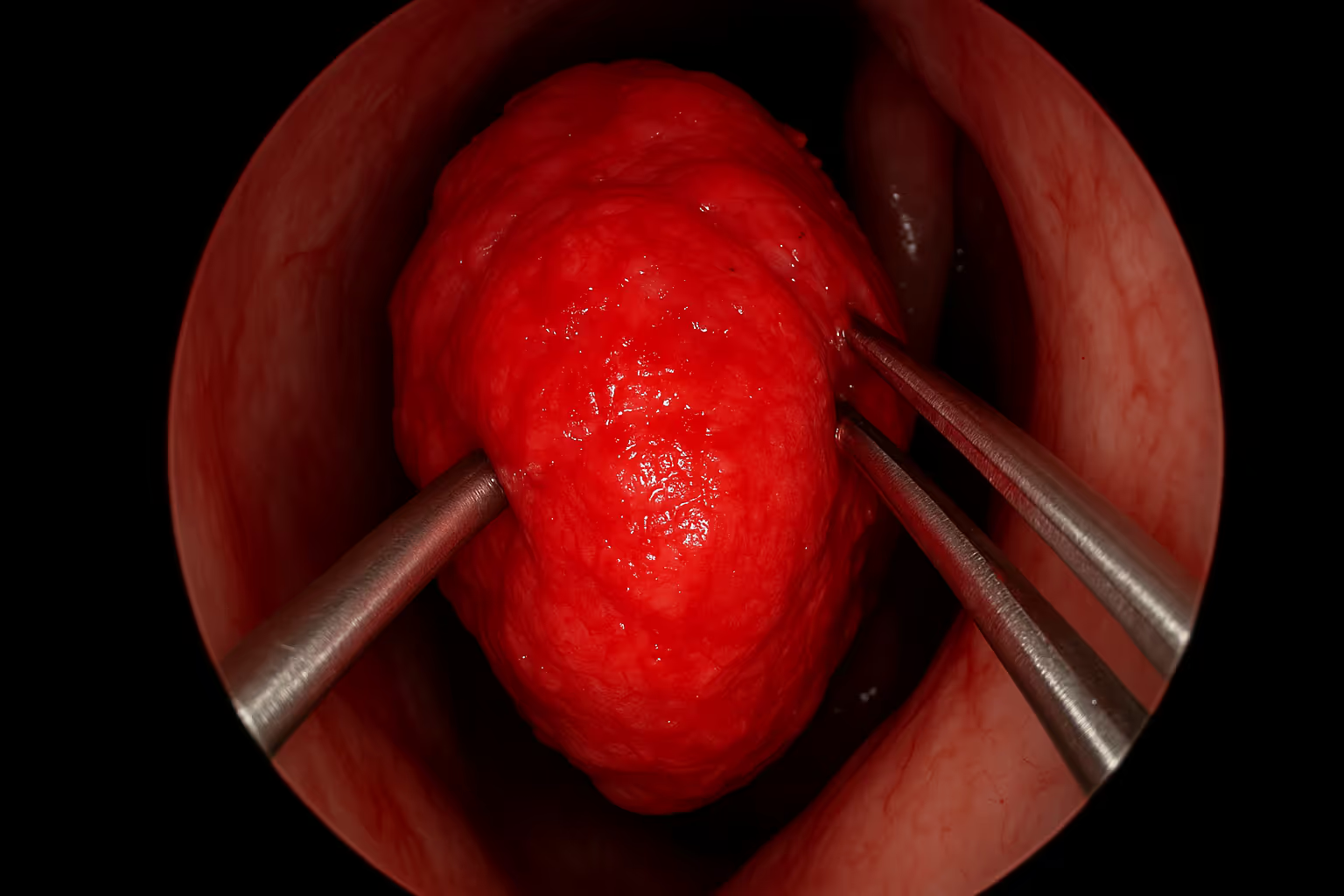
The condition primarily manifests as highly vascular growths that develop almost exclusively in the nasopharynx—the upper part of the throat behind the nose. What makes angiofibroma particularly challenging is its ability to grow into surrounding structures including the sinuses, eye socket, and even the skull, despite being technically benign [2].
Angiofibroma accounts for only 0.05-1% of all head and neck tumors, making it an exceptionally rare condition that many healthcare providers may encounter only a few times throughout their careers [1]. This rarity contributes to the complexity of diagnosis and treatment, as clinical experience with the condition remains limited even among specialists.
The most well-studied and clinically significant type, JNA predominantly affects adolescent males between ages 10-20 years. However, medical literature has documented rare cases in females, representing approximately 12.5% of all reported cases [2]. These female cases present with identical clinical and imaging features, including the potential for orbital and intracranial extension.
This rare benign variant can occur in unusual locations such as the paratesticular region and generally carries a good prognosis when properly treated [3]. CAF represents a distinct pathological entity with different treatment considerations compared to JNA.
Associated with Tuberous Sclerosis Complex (TSC), facial angiofibromas present unique challenges and are currently the subject of ongoing clinical trials for targeted therapies [4]. These lesions typically appear as small, red bumps on the face and require specialized dermatological management.
Interestingly, angiofibromas arising from locations other than the nasopharynx—such as the nasal septum, ethmoid, or turbinate—appear to be clinically distinct and disproportionately affect women [2]. This gender distribution difference suggests varying underlying mechanisms for tumor development based on anatomical location.
The clinical presentation of angiofibroma varies depending on the tumor's location and size, but several key symptoms consistently emerge:
Nasal and Respiratory Symptoms:
Advanced Symptoms:
The rarity of angiofibroma often leads to delayed diagnosis, as initial symptoms may be attributed to more common conditions like allergies, sinusitis, or typical adolescent nosebleeds. Healthcare providers should maintain a high index of suspicion when encountering persistent unilateral nasal symptoms in young males.
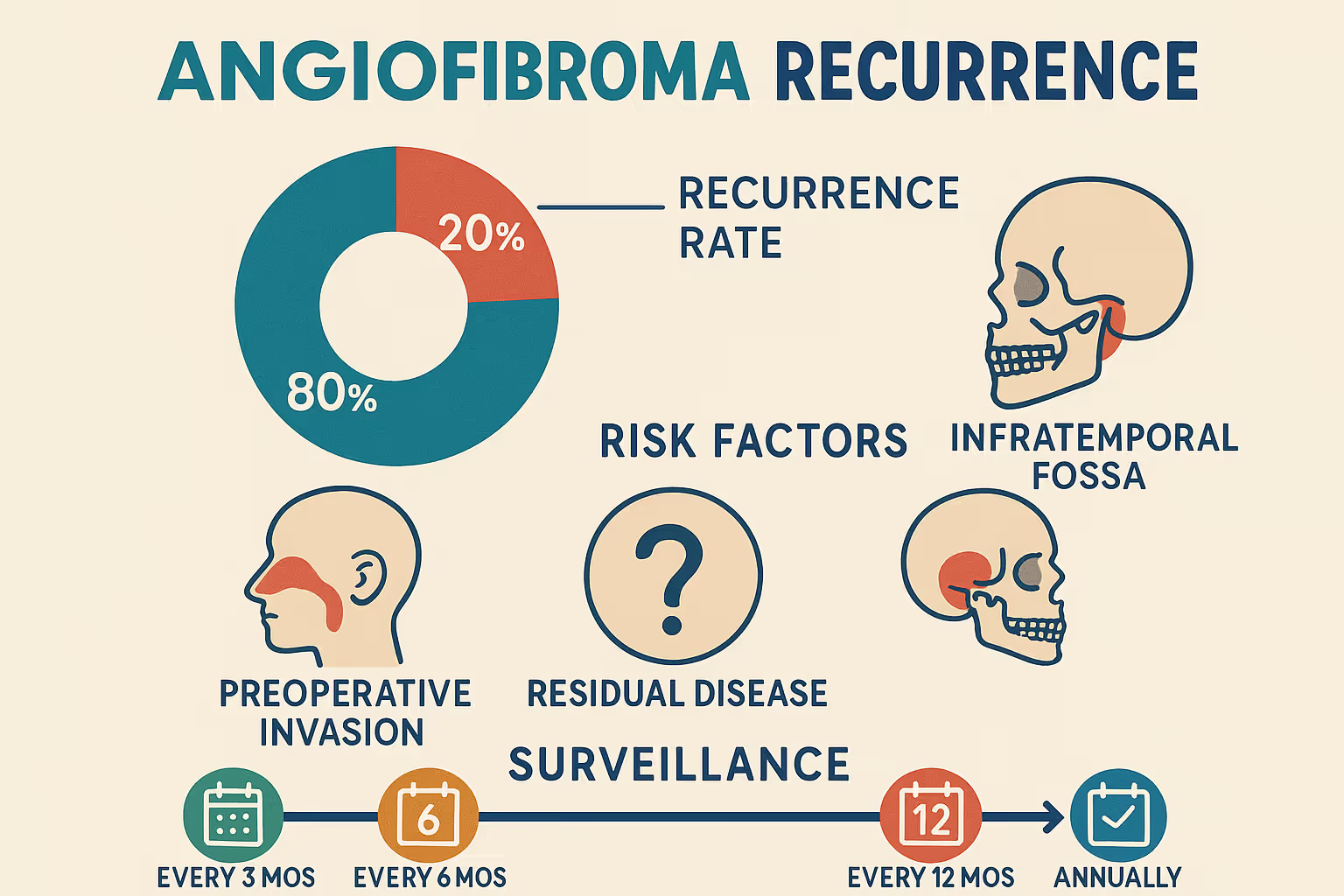
One of the most concerning aspects of angiofibroma is its substantial recurrence rate of 38.2%, based on recent analysis of 68 patients [1]. The mean interval to recurrence was 16.7 ± 14.9 months, with 57.7% of recurrences occurring within the first year after primary tumor excision [1].
Perhaps most alarming is that 61.53% of recurrent cases were discovered incidentally through routine follow-up examinations or imaging, with patients showing no symptoms at the time of recurrence diagnosis [3]. This finding emphasizes the critical importance of systematic postoperative surveillance.
Tumor Size Impact:
Staging Considerations:
Preoperative Embolization: While used to reduce intraoperative bleeding, patients who underwent embolization had a mean recurrence interval of 12 months compared to 31 months for those who did not receive embolization [1].
Blood Transfusion: Perioperative blood transfusion correlated with shorter recurrence intervals (12 months versus 22 months) [1].
Multivariate analysis revealed that age at presentation and primary tumor size were the only independent predictors of angiofibroma recurrence [3]. This suggests that while multiple factors correlate with recurrence, these two variables have the most significant independent influence on treatment outcomes.
Understanding recurrence patterns is essential for surgical planning and follow-up protocols. Research has identified specific anatomical locations where recurrent disease most frequently occurs:
Anatomical SiteRecurrence FrequencyPterygoid process92.3%Nasopharynx84.6%Sphenoid sinus76.9%Maxillary sinus61.5%Ethmoid sinus53.8%
The pterygoid process emerges as the most critical area, being involved in over 90% of recurrence cases [3]. This finding suggests that meticulous surgical attention to this region is crucial for reducing recurrence incidence.
The diagnostic process begins with a thorough clinical history and physical examination. Healthcare providers should pay particular attention to:
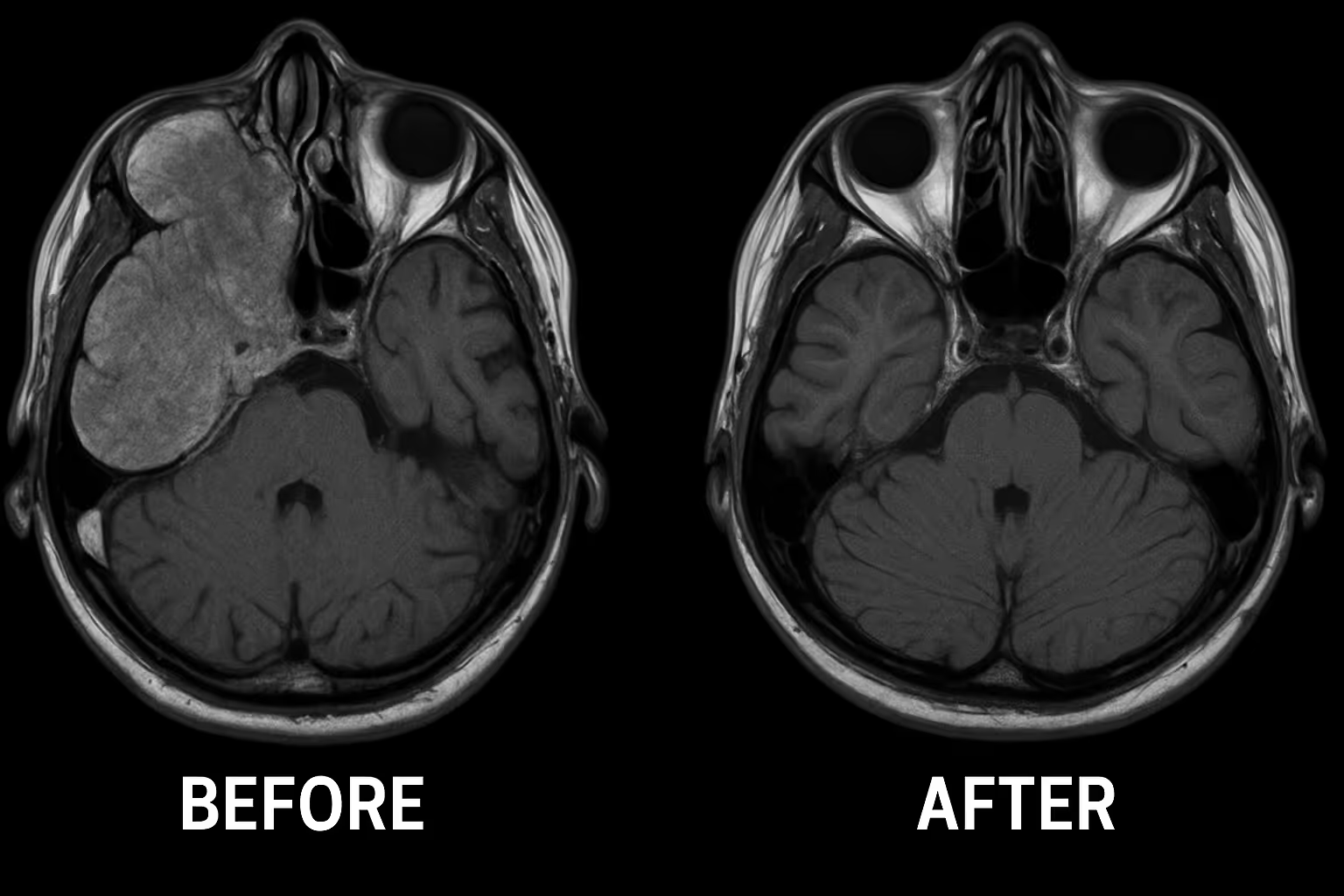
CT Scanning:
MRI Imaging:
Angiography:
While imaging provides crucial information, tissue diagnosis remains the gold standard. However, biopsy of suspected angiofibroma requires extreme caution due to the risk of severe hemorrhage. Many specialists recommend proceeding directly to definitive treatment based on characteristic imaging findings in appropriate clinical contexts.
Endoscopic Resection: Modern endoscopic techniques have revolutionized angiofibroma treatment, offering several advantages:
Open Surgical Approaches: For extensive tumors with significant intracranial extension, open approaches may be necessary:
Embolization: Despite its association with shorter recurrence intervals, preoperative embolization remains valuable for:
Multidisciplinary Planning: Successful treatment requires coordination between multiple specialists, and patients benefit from care at specialized surgical centers with experience in complex vascular procedures.
Radiation Therapy: Reserved for recurrent cases or tumors deemed surgically unresectable:
Medical Therapy: Research into systemic treatments continues:
Given the high rate of asymptomatic recurrence, rigorous follow-up protocols are essential:
First Year (Critical Period):
Years 2-5:
Long-term Follow-up:
Patients and families should be educated about potential recurrence symptoms:
While rare, angiofibroma in females requires special consideration:
Treatment in younger patients involves additional factors:
Patients with associated genetic conditions like TSC require:
The complex nature of angiofibroma treatment involves significant costs:
Patients can explore cost estimation tools to better understand potential expenses and plan accordingly.
Most insurance plans cover angiofibroma treatment as medically necessary, but patients should verify:
Active research focuses on several promising areas:
Intraoperative Navigation:
Advanced Imaging:
Patients and families benefit from comprehensive education about:
Connecting with other affected families provides valuable support and shared experiences. Many patients find helpful resources through specialized medical centers that maintain patient support programs.
Long-term management focuses on:
Seek urgent medical evaluation for:
Schedule regular appointments for:
Patients can find qualified specialists through specialized medical centers with experience in angiofibroma management.
Currently, no proven methods exist for preventing angiofibroma development, as the exact causes remain unclear. However, research continues into:
Focus on preventing complications and recurrence:
No, angiofibroma is a benign (non-cancerous) tumor. However, its locally aggressive behavior and tendency to invade surrounding structures make it a serious condition requiring prompt treatment.
Angiofibroma does not metastasize (spread) to distant body parts like cancer. However, it can grow into adjacent structures including sinuses, orbit, and skull base.
The exact cause remains unknown, though research suggests:
Recovery varies based on surgical approach and tumor extent:
For more detailed information about recovery expectations, patients can consult resources available through specialized treatment centers.
Angiofibroma represents a challenging but treatable condition that requires specialized medical expertise and long-term commitment to surveillance. While the high recurrence rate of 38.2% and potential for aggressive local growth make this a serious diagnosis, advances in surgical techniques, imaging technology, and understanding of risk factors have significantly improved outcomes for patients.
Key factors for successful management include:
✅ Early recognition and diagnosis by experienced healthcare providers
✅ Treatment at specialized centers with multidisciplinary expertise
✅ Complete surgical resection with attention to high-risk anatomical areas
✅ Rigorous long-term surveillance protocols, especially during the first year
✅ Patient and family education about recurrence signs and symptoms
The rarity of angiofibroma makes it essential for patients to seek care from specialists familiar with the condition. The complexity of treatment and high recurrence risk underscore the importance of ongoing research into better treatment modalities and surveillance strategies.
If you or a loved one is experiencing symptoms suggestive of angiofibroma, take these important steps:
Remember that while angiofibroma presents significant challenges, appropriate treatment and surveillance can lead to excellent long-term outcomes. The key is working with experienced healthcare providers who understand the unique aspects of this rare but important condition.
For additional questions about angiofibroma or to explore treatment options, consider reviewing frequently asked questions or consulting with qualified specialists who can provide personalized guidance based on individual circumstances.
[1] Recent analysis of 68 patients with juvenile nasopharyngeal angiofibroma recurrence patterns and outcomes. Journal of Otolaryngology, 2025.
[2] Gender variations in angiofibroma presentation and management. International Journal of Pediatric Otorhinolaryngology, 2024.
[3] Multivariate analysis of risk factors for angiofibroma recurrence. Head and Neck Surgery, 2024.
[4] Cellular angiofibroma: Clinical characteristics and treatment outcomes. Pathology International, 2025.
[5] Tuberous Sclerosis Complex and associated facial angiofibromas: Current treatment approaches. Dermatologic Surgery, 2024.